According to the latest data from the U.S. Centers for Disease Control and Prevention (CDC), about 3.4 million people have epilepsy—two or more seizures not caused by another condition. For some patients, epilepsy surgery or an implanted device can significantly reduce the number and severity of a patient’s seizures.
Epilepsy looks different for every patient because there are many causes and everyone’s brain is unique. In general, epilepsy falls into two main categories:
- Generalized epilepsy: Seizures affect cells on both sides of the brain at the same time.
- Focal epilepsy: Seizures are contained to one area or one side of the brain.
UNM Health Sciences Center provides comprehensive care for all types of epilepsy. As New Mexico’s only National Association of Epilepsy Centers Level 4 Epilepsy Center, we begin with detailed testing to understand where each patient’s seizures start and the specific functions of that part of their brain.
State-of-the-art Imaging and Diagnosis
In addition to a detailed history and conversations about each patient’s history, lifestyle and symptoms, our expert epileptologist often offers various testing to make a diagnosis and treatment plan.
Out first line of management will be anti-seizure medication, based on patient’s history, other comorbidities and basic seizure work up (mostly EEG and MRI brain). If patients do not remain seizure free (refractory epilepsy cases) with trail of two adequately chosen and well tolerated anti-seizure medication, then we offer them phase I (non-invasive) evaluation, which includes work up for possible epilepsy surgery, neuromodulation and/or diet therapy (keto/low carb diet).
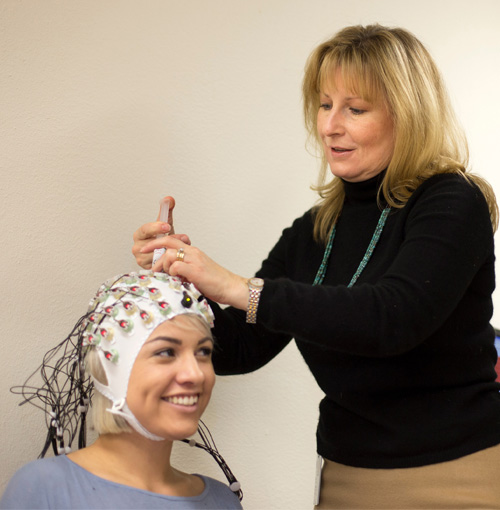
Phase I/non-invasive workup often begins with inpatient video electroencephalograph (EEG) monitoring. Patients stay in private rooms for 3-5 days, while the EEG records the brain’s activity during the moment of a seizure and in between. Doctors analyze the recordings to classify seizures as generalized or focal and identify their origin in the brain.
We also rely on imaging such as high-resolution seizure protocol MRI (often 3 Tesla), functional MRI, PET scan and magnetoencephalography (MEG) to get the most detailed understanding of patients’ seizure network and a baseline of the patient’s normal brain function.
Patients also meet with a dedicated epilepsy neuropsychologist and/or psychiatrist to understand their baseline brain function and manage any psychiatric comorbidities, such as anxiety, that may arise from treatment.
After gathering these data, we hold an epilepsy surgery conference, where our epilepsy team—including all our adult and pediatric epilepsy faculty, epilepsy neurosurgeon, neuroradiologist and neuropsychiatrist—meet to discuss each patient’s seizure details, test results and EMU/EEG seizure videos to plan for next options, including phase II evaluation (stereo EEG, subdural grid/strip) for surgical and neuromodulation planning vs direct surgery.
Then we meet with the patient to put their plan into action. Often, epilepsy fellows partner with our epileptologists to work with patients every step of the way, from presurgical examinations through treatment and postsurgical follow-up.
Related reading: What to Expect in a One-Year Epilepsy Fellowship
Neurostimulation Devices and Surgical Treatment
Many of our patients who have had surgery or received a device are now completely seizure-free or experienced significant seizure reduction. After successful surgical outcome, they can stop medications and return to activities like driving, work, and education. Some of our patients are even enrolled in medical school and law schools!
Generally, neurostimulation devices have been shown to offer patients 50-75% reduction in seizures over time. Surgery can reduce seizures by 60-90%, depending on location and underlying pathology.
Treatments for Generalized Epilepsy
Neurostimulation devices to treat generalized epilepsy include:
- Vagus nerve stimulation (VNS): This device sends a mild electrical pulse through the vagus nerve to the brain, similar to the way a pacemaker regulates the heart. It is implanted under the skin of the chest on left side and connected to the vagus nerve in the neck.
- Deep brain stimulation (DBS): This device sends electrical pulses through wires to the brain. It is implanted in the chest muscle, with electrodes placed near the center of the brain (thalamus). These electrical pulses block signals from nerve cells that trigger a seizure.
UNM Health Sciences Center is participating in a clinical trial of a new device implanted in the thalamus that could help reduce seizures.
For some patients with generalized epilepsy, brain surgery offers the best chance at a significant seizure reduction. Procedures can include:
- Corpus callosotomy: A procedure that splits the main connection between the two sides of the brain so seizures can’t spread.
- Functional hemispherectomy: This surgery prevents seizure spread to nearby areas.
- Anatomic hemispherectomy: Removal of the lobes on one side of the brain, leaving other brain structures intact. This surgery is rarely done and usually reserved for severe epilepsy, in which seizures cause falls, head injuries, and bleeding.
Treatments for Focal Epilepsy
Focal resection surgery is the ultimate cure for most focal seizures, if the seizure focus/location is respectable. In this procedure, the surgeon removes the part of the brain where seizures begin if that area is a non-critical part of the brain. For some patients with focal epilepsy, hemispherectomy can also provide seizure relief.
Neurostimulation devices to treat focal epilepsy include VNS, DBS, and responsive neurostimulation (RNS). The RNS device is implanted within the skull near the site of focal seizures focus and connects to electrodes placed over the skull. RNS devices monitor brainwaves to detect abnormal activity near the seizure focus and deliver brief electrical stimulation to prevent and/or stop a seizure.
For both generalized and focal refractory epilepsy, we also offer ketogenic diet/low carb therapy as inpatient or/and outpatient.
A Chance to Become Seizure-free
The thought of brain surgery or an implanted device can be intimidating for some patients, but we see excellent results and these procedures are very safe and well-planned. We complete all phase I & often phase II monitoring to confirm the location and function of the part of the brain which starts seizure (focus). We only operate when we know we will not impact important brain functions like memory, cognition and language processing.
Explore your options for epilepsy training. Schedule a call with Alexis Gonzalez and JJ Maloney, Medical Education Program Manager for the UNM HSC Department of Neurology. Book now.