At the Clinical Neurosciences Center (CNC) Neurology Clinic, we recently took steps to weed out inefficiencies and improve processes that were eating up valuable time.
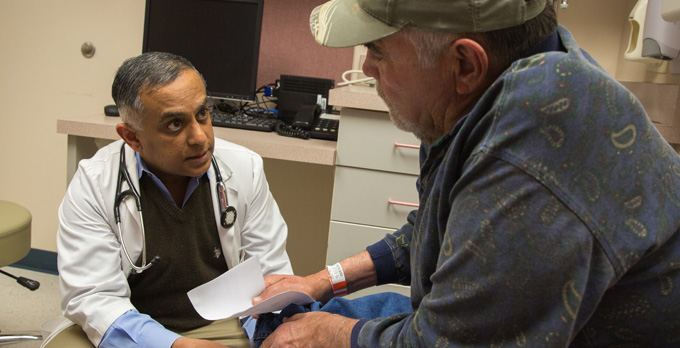
We wanted our providers to have more one-on-one with their patients, and most importantly, we wanted to give patients their time back—no one wants to sit in an empty exam room for 30 minutes waiting to see their doctor.
Increasing clinical face time between patients and providers builds stronger bonds and improves patient outcomes, but it’s not an easy task. With most physicians spending just 27% of their day with patients, there were plenty of inefficiencies to be identified and carved out—we just needed to look in the right place.
The solutions we landed on were dynamic and flexible. They weren’t based on following a spreadsheet of set ratios and schedules, because the flow of clinical care is more complex than that. The changes we made allowed us to maximize our space, which made our clinical services more efficient and increased the quality of care we can provide for our patients.
New Logistics for an Old Problem
At the CNC Neurology Clinic, we care for patients with epilepsy, neuromuscular disorders, multiple sclerosis and other neurological diseases, including after stroke. Building solid relationships with our patients requires providers to feel empowered to take their time with each visit. The key to making this possible is ensuring the clinic is running as efficiently as possible.
When I first joined the team, we had several open RN and MA positions, multiple providers seeing patients and not enough rooms to see them in; we had to really rethink the flow of the unit. We had to figure out how to meet our providers at a healthy pace to allow them optimal face time with their patients and to care for more people who needed our neurology expertise.
I was convinced we could find a way to better coordinate the flow of patients through the clinic—but what was the best solution? To assist us in making and implementing changes, CNC leadership teamed up with the Lobo Quality Improvement Process (LQIP).
Rethinking Space and Time
We ended up altering our processes in two major ways: changing how providers and patients were assigned to rooms and modifying the provider-medical assistant (MA) work relationship.
Math Problems
Previously, our workflow had each provider assigned to two specific rooms—on a good day, the two rooms closest to their work area. While this setup was very logical, it was masking some inefficiencies and making it appear as though our exam rooms were at maximum capacity throughout the day.
However, this way of assigning rooms didn’t account for cancelations or the real-time ebb and flow of patients visiting the CNC. When these factors—and Occupational Safety and Health Administration requirements—were considered, it turned out that each provider only needed approximately 1.25 rooms, not 2.
I knew whittling down 2 rooms to approximately 1.25 rooms would take a whole new approach, so I looked to other clinics for ideas. I found the most plausible solution from observing how the 5th Floor Ambulatory Care Center (5ACC) organized their workflow, and I tailored it to better fit CNC Neurology Clinic. Our room assignments became “first come, first room”.
Exam Room Reassignment
First, we changed the way we assigned exam rooms and the discharge process, which required us to adjust the structure of our team. That meant creating two outpatient clerk positions to run the discharge desk and three Patient Care Coordinators (PCCs) to help with the administrative side of clinic flow. Since the provider would regularly be the last person with the patient prior to discharge, we saved the time of everyone in the clinic by having the provider print the visit instructions and walk the patient to the discharge desk. This meant the MA or RN could clean the room while the provider walked the patient to the discharge desk, making it immediately ready for their next patient.
With these staff and flow changes in place, we adjusted our process so that patients would be roomed in any exam room that was available. Providers no longer had assigned rooms. There was concern that this process would make it harder for providers, but in practice, they were more likely to have their patients roomed near their work areas and roomed faster because there was always an open, clean room ready for the patient. This flexibility opened up space and allowed us to hire more providers to see more patients.
Relationship Routines
Next, we switched up the way our MAs and providers worked together. This change required some trial and error. We initially tried having the MAs room for any provider; however, we found that this system made it difficult for providers to keep track of which MA had roomed their patient, creating inefficiencies in getting more information or answers to questions.
So, we started assigning MAs to specific providers within a subspecialty so the same providers and MAs would work together day after day, streamlining clinical interactions. This MA-provider relationship aided communication because the provider always knows who they need to connect with if they have questions or if they want to run additional tests.
Working with assigned providers allowed the MAs to learn their preferences. For example, if an MA knows their provider is particularly concerned when anyone’s diastolic blood pressure is less than 70, that MA will automatically recheck a sub-70 diastolic without waiting for the provider to request it. Small efficiency improvements lead to better patient care over time.
Succeeding as a Team
Merely instating a new process, no matter how wonderfully efficient it is, will not usher in success. The crux of a positive outcome is having a team with the right attitude. The CNC is open to new ideas, willing to learn from others and can endure the pains of adaptation for the greater good. It helps that the team has been through a lot together and we’re very supportive of one another.
We also have real partnership among our providers—it’s not a power struggle because they understand the best way to care for our patients is to come together to open access for all.
Another advantage we have in this unit is our incredible team of nurses and MAs, several of whom worked in the Neurosciences ICU at the peak of the COVID-19 pandemic and appreciate what being more efficient with time can mean for staffing.
We were incredibly lucky to be able to hire amazing staff from within the organization and find a perfect fit for those who loved neurology nursing but needed a break from the challenges that come with working in the ICU. They joined the CNC refreshed and ready to help tackle inefficiencies.
Rewarding Outcomes for Patients and Providers
We’ve seen some impressive outcomes since we made these logistical changes:
- We have decreased the average amount of time in which a patient is not engaged with a staff member or provider from 39 minutes to 12 minutes—that’s a half an hour we can turn into facetime between patients and providers.
- We went from having zero available rooms to having 7 to 17 available rooms, depending on the session.
- Our providers appreciate the improvements—their patients are roomed faster and the flow is more organized.
- Communication has improved between staff and providers. It feels as though we have deepened our professional relationships as a team.
- Amid all the turmoil the healthcare industry has been facing recently, we’ve been able to maintain consistent, appropriate staffing.
Looking Forward to Superior Care
Now that we’ve opened space for more specialists, we hope to bring on doctors who share our values and attitudes toward patient care—namely those who are willing to embrace a few growing pains when it means offering superior care to our patients.
At the same time, we aim to build a team that appreciates the value of everyone’s expertise, and we’ll put in the work to ensure every minute counts. We aim to set the stage for future neurologists and encourage an attitude of challenging clinical situations perceived as “good enough” while always working toward better clinical experiences and patient outcomes.
In summer 2023 we plan open a Headache Clinic, and we look forward to implementing the most efficient processes there, too. We’ll continue to adopt practices that improve patient care and make workflows better for our providers and staff members. I feel fortunate to work with a CNC team that has an open-minded attitude that makes these improvements possible.