More than two years into the global pandemic, post-acute sequelae SARS-CoV-2 infection, or long COVID, continues to bring patients to the clinic, hospitals and intensive care unit with a myriad of multi-systemic symptoms.
Long COVID is the umbrella term for COVID-19 symptoms that arise or persist three months or longer after being infected with the virus. Approximately, 1 in 13 U.S. adults has systemic long COVID symptoms that can affect the brain and heart, digestive or respiratory systems.
Research published in JAMA Network details neurological complications that COVID-19 can cause acute emergencies, including:
- Stroke
- Seizures
- Intracerebral hemorrhage
- Cerebral venous sinus thrombosis
- Meningitis
- Acute encephalopathy
- Coma
Further, COVID-19 may also cause symptoms over days to weeks, such as difficulty thinking or concentrating (sometimes referred to as “brain fog”), headache, sleep problems, dizziness, lightheadedness, pins-and-needles feelings, change in smell or taste, anxiety or depression that can persist for a prolonged period.
Timely detection and treatment for COVID-19, long COVID and their neurological symptoms can help patients recover more successfully in the setting of neuro-emergencies. UNMHSC and UNM Department of Neurology are equipped with state-of-the-art technology, equipment and resources that complement a diverse group of neurological specialists who can help in these emergencies. We are the state’s only Comprehensive Stroke Center and Neurological Institution, and we can provide care for such complex cases.
Further, UNMHSC’s Clinical Neurosciences Center can assist with symptoms related to long COVID in a non-emergent setting. Clinical Neurosciences Center encompasses multiple subspecialities including epilepsy, movement disorders, sleep medicine and cognitive neurology amongst others.
Across the U.S., researchers at the National Institute of Health’s RECOVER initiative and the CDC’s INSPIRE project are working to understand the effects and potential treatments for long COVID. UNM Health Sciences Center is leading two specific projects are helping doctors learn more about long COVID:
- The gut-brain connection in long COVID
- COVID-19 neuropsychological dysfunction
There are no specific treatments for long COVID, and the condition affects each patient differently. So, we take a team approach to personalize care for each patient and help improve their health.
Let’s discuss how long COVID can affect the brain and body, what we can do to relieve its symptoms, and how we’re adding to the body of research to help more patients avoid or manage the condition.
Neurological Symptoms of Long COVID
Though long COVID is more common in people who had a severe case of COVID-19, even people who had a mild case can develop chronic symptoms. Some long COVID symptoms go away and return later, and while most patients notice symptom improvement over time, some cases last for months and can result in disability.
There is no specific test for long COVID. In general, people with long COVID report running a fever and experiencing fatigue that interferes with their daily life. These symptoms often get worse after strenuous mental or physical work.
Long COVID can be systemic, meaning it affects different areas of the body. Brain is one of the most important organs affected by COVID-19 which can cause disabling symptoms that linger for weeks to many months. If you notice any of the following symptoms after recovering from COVID-19, call 505-272-4866 to schedule a visit with a doctor.
Neurological and cognitive symptoms can include:
- Anxiety or depression
- Brain fog (difficulty thinking or concentrating)
- Changes in your sense of smell or taste
- Feeling pins and needles
- Headache
- Lightheadedness
- Mood changes
- Trouble sleeping
Diagnosing and Treating Long COVID
It’s common for people with long COVID to have symptoms that are difficult to explain or measure. Diagnostic tests such as X-rays, EKGs and blood tests can appear normal, making diagnosis difficult. Patients and providers must keep open lines of communication to understand the patient’s condition and connect them with appropriate care.
There is not yet a recommended treatment for long COVID. However, one fact is clear—vaccination is the best way to avoid getting COVID-19, and subsequently is our best defense against long COVID.
UNM Health Sciences Center providers coordinate holistic, team-based care to help patients manage their symptoms. This can include methods like physical therapy or cognitive therapy to manage symptoms such as anxiety and depression. Your doctor may refer you to a specialist, such as a respiratory therapist or gastroenterologist to help manage specific symptoms.
It is important for patients and caregivers to find support and understand they are not alone in their struggle. Organizations like the Long COVID Alliance and Survivor Corps offer advocacy for patients and referrals to support groups.
As our global society begins to recover from the devastating impacts of the COVID-19 pandemic, ongoing research will help us understand how best to manage this long-term condition.
Related reading: UNM COVID Analytics and Reporting
Ongoing research to understand long COVID
Researchers at UNM Health Sciences Center participate in efforts to the many questions surrounding long COVID. We are currently involved with three studies specifically to understand systemic effects of long COVID.
NIH RECOVER: Researching COVID to Enhance Recovery. This is a multicenter study created by NIH to learn about the long-term effects of COVID. UNM HSC partners with other institutions and bring our own expertise to this important research that aims to understand how people recovery from COVID infection and why some people do not fully recovery and develop Long COVID or PASC (post-acute sequelae of SARS-CoV-2).
Gut-Brain Research
Through our longstanding partnership with The MIND Research Network, principal investigator Andrei Vakhtin, PhD, is leading a study called “Gut-brain axis etiology of post-acute COVID-19 syndrome in older adults” to examine whether an imbalance in the digestive microbiome or permeability between the digestive system and bloodstream might expose the brain to neuroinflammatory substances, resulting in chronic neurocognitive impacts from the virus.
The gut microbiome can secrete potent neurotoxins that affect the functioning of the neurological system. When these toxins get into the bloodstream, the result can be unexplained symptoms such as brain fog and memory lapses.
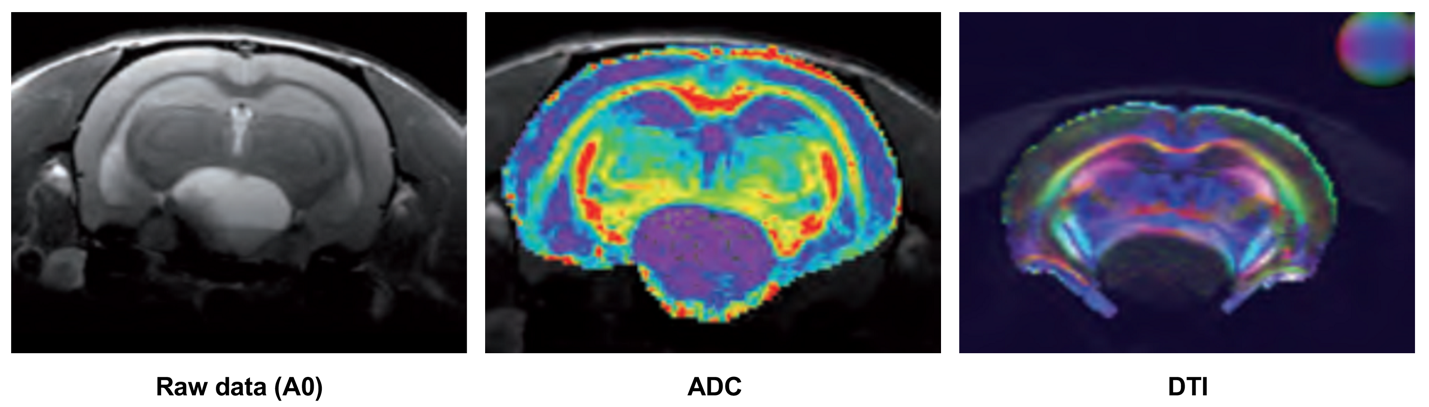
To seek out the cause of neurological inflammation, researchers are innovating new uses for magnetic resonance spectroscopy (MRI) and diffusion imaging to learn how metabolites in the brain diffuse in brain tissue in adults age 56 to 75 who have had COVID-19. The study is currently enrolling participants. To learn more, call 505-226-2609.
Neuropsychological Research
At our the Center for Brain Recovery and Repair, principal investigator Davin Quinn, MD, is leading a team of researchers and trainees to expand our understanding of long COVID’s effects on the brain.
The study, “Investigating mechanisms of COVID-19 neuropsychological dysfunction,” uses imaging such as electroencephalography (EEG) to study the brain’s electrical activity and functional near infrared spectroscopy to measure blood flow in the brain. These tests are supported by traditional neuropsychological assessments.
The goals of this study are to determine whether:
- Long COVID increases or decreases the brain’s electrical functioning and blood flow
- Chronic objective cognitive problems such as brain fog and memory problems can be uncovered through corresponding neuropsychological testing
- Asymptomatic COVID-19 infection can lead to long COVID
The study is enrolling patients who have long COVID, those who had COVID-19 with no long COVID symptoms, and thos who have never had COVID. To find out how to enroll in this study, email Jude Chavez, Clinical Research Supervisor at 505-272-4411.
While many questions remain about the COVID-19 virus and its long-term effects, researchers around the world will continue to seek answers. As patients, providers and scholars in our global community, we must all do our part to get vaccinated and boosted, contain the spread of the virus and reduce the risks of long COVID complications.