A Successful Year
[NCI] Comprehensive designation is a testament to the world-class quality of our clinical and research programs. — Alan E. Tomkinson, PhD

Dr. Dayao was my medical oncologist. She really helped guide chemo and my overall treatment path. She is definitely who I see as the quarterback of my team. — Elyse Eckart, Patient

I am passionate about optimizing healthcare facilities management. While I may not be directly treating patients, I know that the results of my team’s successes can make the experience of a patient better. — Stewart Livsie

Embracing Complexity
Dr. Ben Ferguson says the complicated challenges posed by cancer care are what drew him to surgical oncology.
READ
MORE

CLOSE
Embracing Complexity
Ben Ferguson, MD, PhD, was drawn to cancer care because it’s complicated.
Dr. Ben Ferguson says the complicated challenges posed by cancer care are what drew him to surgical oncology.
“I got involved in cancer research as a medical student and really fell in love with some of the problems that the field of cancer care faced and was intrigued by the intersection of research questions and clinical questions,” Ferguson says. “That really put me on the track of wanting to be a physician that treats cancer patients.”
It wasn’t always this way. Ferguson grew up in Chicago and is the son of two physicians. His father is a thoracic surgeon and his mother is an anesthesiologist. In his youth, Ferguson says, he tried to avoid following in his parents’ footsteps. But by the time he was in college, scientific questions began to fascinate him.
“Despite my best efforts to avoid it, I really realized the science was something I was interested in,” Ferguson says. “And medicine provided the best way I could tell at the time to do something with that science knowledge in terms of making an impact on certain people’s lives.”
Ferguson joined the University of New Mexico, School of Medicine and the UNM Comprehensive Cancer Center as a surgical oncologist in August.
He completed a fellowship in complex general surgical oncology at the Memorial Sloan Kettering Cancer Center in New York from 2018 to 2020. Prior to that, Ferguson completed a residency in general surgery, including one year as an administrative chief resident, at the University of Chicago, Department of Surgery.
Ferguson also completed his MD, a PhD in cancer biology and a Medical Education Research, Innovation, Teaching and Scholarship fellowship at the University of Chicago.
He received his Bachelor of Science in molecular and integrative physiology from the University of Illinois at Urbana-Champaign.
“I was inevitably drawn to surgery based on the exposure I had from my parents, but I was intrigued by it for the basic reason that it tends to provide patients with somewhat immediate results,” Ferguson says.
Ferguson said he felt no pressure to get into surgery and to some extent was encouraged to look at other options because of the time commitment it requires.
The complexity of problems cancers pose drew his attention, and the collaborative approach to treating cancers also fascinates him.
“From biochemistry to immunology to certain aspects of microbiology – all of those are in some interplay,” he says.
“It was a bit of good luck in the sense that this University was looking for a surgeon that overlapped quite a bit with my clinical interests and my research interests,” he says. “Once I arrived, I really fell in love with the city and surrounding environment. Since arriving, I’ve found it to be a very easy place to live, with happy neighbors.”
Ferguson said the UNM Comprehensive Cancer Center is a draw because of its designation as a National Cancer Institute comprehensive center, the highest endorsement available from the NCI.
The designation, he says, gives UNM credibility among patients and providers and ensures that resources are available to physicians working at the center.
But Ferguson said he also likes the relatively small size of UNM and the Department of Surgery, because it means he will have plenty of opportunities to stay busy.
“The state of New Mexico has a somewhat unique patent population, in that there is a fairly high rate of somewhat rare cancers, especially liver and gallbladder cancers,” Ferguson says. “Some of these are diseases that interest me, so it’s a good opportunity to become involved in their care.”
The UNM Comprehensive Cancer Center also provides strong opportunities for research and clinical trials and the potential to collaborate with other physicians and research scientists, Ferguson says, adding that he has a strong background in research in which he has collaborated with medical oncologists, biostatisticians and epidemiologists.
Ferguson says he would like to treat cancers of the stomach and esophagus and also is interested in surgical education. He is serving as the associate Program director of the complex general surgical oncology fellowship at the UNM Comprehensive Cancer Center, which received its first fellow this year.
While a move from the big cities of New York and Chicago to Albuquerque might bring a degree of culture shock, Ferguson said there’s plenty of upside to the Duke City.
“The weather is much better here,” he says. “The opportunities for outdoor activities are much better here. The cost of living is much better here. I think the overall attitude of the population is much better here.”
At UNM Cancer Center, Ferguson will focus on treating cancers of the liver, pancreas and bile ducts.
A Measure of Cleanliness
READ
MORE
UNM Cancer Center Scientist Develops and Validates a Method to Test Surfaces for Virus Particles



A Measure of Cleanliness
February 8, 2021
CLOSE
UNM Cancer Center Scientist Develops and Validates a Method to Test Surfaces for Virus Particles
Doctor’s offices and hospitals meticulously clean the nondisposable medical equipment they repeatedly use. Equipment that cannot be heat-sterilized must be cleaned with powerful disinfectants. Michelle Ozbun, PhD, an international expert on viruses, wanted to know how effective those disinfectants really are.
Ozbun and her team developed a way to measure how many infectious human papillomavirus particles are left on a surface after it has been disinfected. They found that disinfectants approved for use on medical devices work well, and they recently published their work online in The Lancet journal EBioMedicine.
Ozbun is a professor of Obstetrics & Gynecology and of Molecular Genetics & Microbiology at The University of New Mexico. Her research focuses on HPV, which causes more than 90% of cervical and anal cancers and more than 70% of vaginal and throat cancers, according to the Centers for Disease Control and Prevention.
She explains that HPV particles, like all viruses, need to invade a cell in order to produce copies of themselves. And to invade a cell, the virus particle’s capsid must be intact.
The capsid is the outer shell of a virus particle. It is made of viral proteins and encloses the virus’s genetic material, which encodes those proteins. Some viruses, called enveloped viruses, have a layer of fat-like molecules covering the viral proteins.
“Coronavirus and HIV and herpesvirus are all enveloped viruses,” Ozbun says. “They’re much more susceptible to drying out on a surface. And if they dry out, they’re not infectious.”
Viruses like HPV, poliovirus and norovirus have capsids made of just proteins, which means they can remain on surfaces for a long time without becoming inactivated, Ozbun says. “And so,” she says, “they’re much harder to inactivate by disinfectants as well.”
Because HPV does not kill cells, the only way to detect its presence — until now — has been to take a sample of cells, grind them up and search the genetic material for the virus’ genes.
“When people in the field look to see if people have HPV,” Ozbun says, “they’re really just detecting the viral genomes that are there. They don’t know [whether] these viral genomes are packaged inside the capsid.” And once the cells have been ground up, counting the number of intact HPV particles becomes impossible.
An additional problem with the grinding method, Ozbun explains, is that the insides of the cells are mixed together. There’s no way to tell if many cells in the sample are infected with a low level of virus products or if only a few cells are infected with a lot of virus products.
Ozbun needed more sensitive methods, so she created them.
First, Ozbun and her team obtained viral samples from three sources. They grew HPV particles in Ozbun’s lab, they obtained HPV samples from another lab, and they collected HPV samples from patients in New Mexico. Next, they infected cells in a lab with the viral samples. But then they did something different: instead of grinding up the cells, they added a stain that binds to viral RNA and took images of the cells.
Ozbun’s images show intact cells with viral RNA inside. Using sophisticated microscopic techniques developed at the UNM Comprehensive Cancer Center, she and her team are able to count how many cells are infected, allowing them to calculate how many virus particles were present.
Using their images and counting methods, Ozbun and her team were able to show that commonly used disinfectants reduce the number of viral particles by at least 10,000 times. They showed that the disinfectants had similar results regardless of the viral source. And they showed that their methods were sensitive over the range of particles that most hospitals and doctors’ offices normally encounter.
Her new method, says Ozbun, “is an important way of differentiating how much nucleic acid is there, versus what’s really infectious. This is the only way that we can tell the number of infectious particles.”
Ozbun explains further that many cleaning procedures call for equipment to be washed before being disinfected. Washing gets rid of many infectious particles before the disinfectant is used.
The result, she says, is that hospitals and doctors’ offices “have an even higher level of confidence that [they’re] not going to expose patients to virus that’s left over from someone else.”
Image: Figures 4c through 4n from the research publication, showing the cells in purple and the RNA as red dots[1].
About Michelle Ozbun, PhD
Michelle Ozbun is a professor in the departments of Obstetrics & Gynecology and Molecular Genetics & Microbiology. She is The Maralyn S. Budke Endowed Professor in Viral Oncology and co-leads the Cellular and Molecular Oncology Research Program at the UNM Comprehensive Cancer Center.
Paper Reference
“Infectious titres of human papillomaviruses (HPVs) in patient lesions, methodological considerations in evaluating HPV infectivity and implications for the efficacy of high-level disinfectants” was published online in January 2021, in EBioMedicine by The Lancet. Authors are: Michelle A. Ozbun, PhD; Virginie Bondu, MA; Nicole A. Patterson, BS; Rosa T. Sterk, BS; Alan G. Waxman, MD; Erica C. Bennett, MD; Rohini McKee, MD; Ankur Sharma, MD; Jeremy Yarwood, PhD; Marc Rogers, PhD; and Gary Eichenbaum, PhD.


Honored Researcher
Dr. Ichiko Kinjyo Receives 2021 Liz Tilberis Early Career Award From the Ovarian Cancer Research Alliance
READ
MORE
CLOSE
Honored Researcher
March 1, 2021
Dr. Ichiko Kinjyo Receives 2021 Liz Tilberis Early Career Award From the Ovarian Cancer Research Alliance
The groundbreaking work being done on ovarian cancer treatment at The University of New Mexico Comprehensive Cancer Center has drawn national recognition and financial support from the Ovarian Cancer Research Alliance.
Ichiko Kinjyo, MD, PhD, a research assistant professor in the UNM Division of Molecular Medicine and at the UNM Comprehensive Cancer Center, was recently named a 2021 recipient of the Liz Tilberis Early Career Award.
Kinjyo was recognized for her work with Sarah Adams, MD, in exploring how a combination of a cancer-targeted agent known as a PARP-inhibitor and immunomodulation via immune checkpoint blockade can improve treatment in patients with ovarian cancers.
PARP-inhibitors are an oral form of chemotherapy that induce cancer cell death by blocking a cell’s ability to repair its DNA. Immune therapy is another new treatment strategy that works by enhancing a patient’s immune response to cancer. Kinjyo’s work has identified the mechanism by which these different approaches can work together for even greater treatment benefit.
Kinjyo’s work under the new grant will focus on how PARP-inhibitors directly affect immune cells, and whether they can enhance the anti-cancer effects of T cells.
“The drug was initially studied by cancer biologists but not by immunologists,” Kinjyo said. “With more and more potential effects of PARP-inhibitors in intracellular regulation, we are interested in the long-term impact on the immune system. That’s the caveat we don’t know yet.”
Adams launched a clinical trial of the combination of PARP-inhibitor and immunotherapy treatment at the UNM Cancer Center in 2016. Once this trial was underway, she recruited Kinjyo to join this work because of her expertise in T cell biology.
“Ichiko is an outstanding scientist,” Adams said. “She is spearheading critical work that investigates how anti-tumor immunity is enhanced by this combination regimen. Her results have already expanded our understanding of the impact of PARP-inhibition in cancer biology and tumor immunology.
“Her new project will test an exciting hypothesis that links immunometabolism, DNA repair and cancer biology and has the potential to significantly impact treatment for women with ovarian cancer and other tumor types.”
Originally from Japan, Kinjyo moved to UNM after completing her PhD work under the mentorship of Akihiko Yoshimura, PhD. She completed postdoctoral training in T cell immunology in the lab of Steven L. Reiner, MD, at the University of Pennsylvania, and subsequently with Dr. Wolfgang Weninger, MD, at the University of Sydney, Australia.
In 2014 Kinjyo joined the lab of Bridget Wilson, PhD, at UNM, where her research focused on acute lymphoblastic leukemia.
Kinjyo chose her career as a basic scientist because of her curiosity about how the body is maintained as a biological system, but said working with a physician-scientist like Adams is a special experience.
“Sarah bridges between clinical bedside and research bench by bringing patients’ wishes to us and reminding us of the demand for better treatments to cure cancer” she said. “We strongly wish to contribute to improving clinical cancer treatment through our daily findings from the lab.”
Kinjyo expects that basic research to uncover the additional effects of PARP inhibitors beyond their impact on DNA repair will enhance treatment efficacy and contribute to the design of new combinations. Her work also has the potential to expand the use of PARP-inhibitors for other types of cancer.
The Liz Tilberis Early Career Awards are given to junior faculty at the assistant professor level who have a strong commitment to an investigative career in ovarian cancer research. The award was started in 2000 and is named for the late-president of the Ovarian Cancer Research Alliance. OCRA was incorporated in 1994 and is the oldest and largest ovarian cancer charity in the world. Since its inception, OCRA has raised over $100 million ovarian cancer research.
Crushing It
READ
MORE
Kyle Stepp overcame a multitude of challenges from bone cancer to remain committed to an active and generous life



Crushing It
March 8, 2021
CLOSE
Kyle Stepp overcame a multitude of challenges from bone cancer to remain committed to an active and generous life
One warm October afternoon in the mountains of northern New Mexico, Kyle Stepp met his destiny.
It was the last run of the day and Stepp was speeding down a mountain bike trail at the Angel Fire Resort when he lost control on a turn and slammed his reconstructed left leg into a tree.
“I hit exactly at the femur where the endoprosthesis was anchored,” Stepp says. “I completely fractured my femur, and the internal prosthetic had separated from my leg. I’m lying there, and I knew the day I had anticipated all these years had finally come. I just felt a sense of peace and calm.”
Stepp made three phone calls while he waited for emergency personnel to arrive and transport him off the mountain.
The first two were to his adoptive mother and brother and the third was to his oncologist, asking her to let the team at The University of New Mexico Comprehensive Cancer Center know that he would soon be arriving at the hospital.
Saving Limbs and Function
The UNM Comprehensive Cancer Center is the only place in New Mexico that offers orthopaedic surgical oncology. The specialty team interacts with a multitude of patients, from those diagnosed with more common forms of cancer, to rare cases like Stepp’s, where the tumor originated within the bones themselves, says surgeon David Chafey, MD.
“If you take all the common cancers – prostate, breast, kidney, lung – up to about 15 percent [of patients] can have manifestations in the bone,” Chafey says. “That doesn’t sound like a lot, but when you aggregate all of those cancers it’s quite a bit. In those patients, their oncologist will continue to treat cancers and find cures. My role is to help them get rid of the pain and stay walking.”
For bone cancers, Chafey is much more involved, but the process can lead to difficult choices for patients.
“The other types of cancer that I treat that are quite a bit rarer than cancers that primarily arise in the bone,” he says. “Kyle is a rare example of childhood bone cancer. In those cases, my role is both to cure the cancer, along with restoring function.”
Because these cancers are rare, cases are evaluated based on tumor size and location and what the cost is to the patient’s quality of life to remove the cancer, Chafey says
“If the tumor is arising from the muscle or bone and you remove that completely, are they going to be left with [a] functional leg that has an option for reconstruction?” he says.
The Hardest Thing to Hear
A few days after the mountain bike accident left Stepp alone in the hospital, he called Chafey and let him know of his decision. The next day, Stepp’s leg was amputated above the knee.
The surgery marked the end to a chapter in the 26-year-old’s life that had begun a dozen years earlier, when he had left a tumultuous childhood for what promised to be a fresh start in Albuquerque with his grandparents.
“I was abandoned as a kid,” he says. “So I, for once, felt like I had a home and a family. I felt like this was a new beginning.”
Stepp planned to walk through the doors of Del Norte High School brimming with confidence and an attitude to try everything. Run for student government. Try out for baseball. Embrace every opportunity that came along.
Then one afternoon during a kickball game in gym class, the ball was kicked directly into his knee. “I just dropped to the ground and started crying. I was just in excruciating pain,” he says.
The solution at the time was to wrap the knee and assume things would be fine.
The next week, during baseball tryouts, Stepp tried to stretch a base hit into a double, slid into second base and felt his knee pop. Again, excruciating pain.
While the assumption was still that it was a sprained knee, Stepp was instructed to visit a family physician to get a closer inspection. When the doctor probed below his left knee, Stepp says the excruciating pain returned and the doctor ordered an X-ray.
“I had no idea what was about to happen,” Stepp says. “That Friday night, the doctor calls my grandparents and shares with them he has concerns and that, ‘We need to get Kyle to UNM Children’s Hospital right away.’”
The X-ray revealed a large tumor in his leg. A biopsy revealed stage four osteosarcoma.
Stuart Winter, MD, a pediatric oncologist at UNM at the time, told Stepp that the cancer also had spread to his lungs. Suddenly, the promise of a new life was transformed into the fight of his life.
“You could sense his calmness,” Stepp says of Winter. “I remember he always wore the coolest bow ties. He said, ‘Kyle I’m going to walk you through the biopsy and the test results,’ and said, ‘Kyle what I’m about to tell you is going to be one of the hardest things you’re ever going to have to hear. But what I want you to know is we’re going to be with you every step of the way.’ Then [he] said the word ‘cancer.’”
Winter reassured him again and they got to work planning out his treatment. In addition to removing the tumor from his leg, Stepp would eventually undergo 18 rounds of chemotherapy.
Stepp traded classmates and teammates for doctors, nurses and, especially, fellow patients in the hospital. The kids bonded over video games and their quiet, shared purpose of fighting cancer.
“I remember Cesar, on my first day, he came in and sat in the chair next to the bed. He handed me an Xbox controller and said, ‘Welcome to the unit,’” Stepp says. “I remember him hanging out with me and we didn’t talk about cancer. There was this unspoken commitment to each other.”
Difficult Choices, Many Factors
Being active and playing outdoors has always been a cornerstone of Stepp’s lifestyle. In the worst times of his childhood, he found solace on the bicycle and the baseball diamond, so the thought, at 14, of losing a leg to cancer was anathema.
After the first half of his chemotherapy treatments was complete, Stepp went into surgery to salvage his leg.
“My femur, knee and tibia were replaced with a stainless steel rod,” Stepp says. “Saving my limb was important because I was self-conscious about who I was at the time.”
Chafey’s predecessor at the UNM Comprehensive Cancer Center performed the surgery. Despite some complications, Stepp was eventually back on his feet.
“Kyle still had to go through chemotherapy, but the surgery was done with a curative purpose, and by all measures, they met that,” Chafey says.
The difficult choice for patients over whether to remove a limb or try to salvage it is influenced by myriad factors, Chafey says. Some patients are older and may have other conditions that would complicate a limb alvage. In other cases, where their cancer originated elsewhere in the body, patients may still be undergoing treatments to battle that.
“Most of the time, it’s driven primarily by their quality of life and goals,” Chafey says. “Removing the bone that’s weakened doesn’t necessarily give patients a better chance at survival. Survival is dictated by their cancer treatment and their treatment response. Surgery won’t necessarily improve that aspect. It will definitely improve their mobility. They can get in and out of the car easier or extend how long can they can walk.”
For cases of bone cancer, patient goals are a factor, as well as the sheer possibility of saving the limb after the tumor is removed.
If the limb can be saved, there are other factors to consider, including increased risk of infection and the fact that the prosthetic won’t last forever.
“I tell patients it’s like keeping the same car you got at 16 and driving it safely because you’re not going to be able to get a new one,” Chafey says. “So, if you drive it hard and put a lot of miles on it, you’re going to start coming up with problems.”
Honoring Childhood Friends
Stepp says he received the same type of advice: Take it easy.
He says he always knew there was a chance his prosthetic might break, and during his junior year at UNM an accident did just that. He was able to get the prosthetic repaired and Stepp made a conscious decision about how he would handle living with a rebuilt leg.
“After that procedure I knew if it breaks again, I was probably going to have an amputation,” he says. “I said, ‘You know what, I’m going to get the most out of this prosthetic.’”
Of the nine core friends he made during his time in cancer treatment, only Stepp has survived.
He carries their memory with him everywhere he goes and tries to honor them with the life he lives.
Cycling became a passion, as did giving back to the community. Stepp got involved with the Lobo Cancer Challenge, a cycling and run/walk fundraiser to support cancer research and treatment at the UNM Comprehensive Cancer Center. As an ambassador and 100-mile rider, he dedicates his personal and team’s fundraising to pediatric cancer research at the UNM Cancer Center.
While he was undergoing treatment in high school, Camp Enchantment, a summer camp for kids fighting cancer, became an annual highlight. In his senior year at UNM, Stepp relaunched the camp as an independent nonprofit and currently volunteers as the president of its board of directors.
He started working for the national headquarters of the Children’s Miracle Network Hospitals.
He remained physically active.
‘No Hesitation, No Reservation’
After his wreck on the mountain in October 2020, Stepp was transported to a hospital under siege by the COVID-19 pandemic. No visitors were allowed and rooms were at a premium. But Stepp says the UNM Cancer Center team never let him feel alone.
“I remember that night after the X-rays, sitting in a room with no windows. But the one bright light in all of this was the team,” Stepp recalls. “Drs. Chafey, Aamir Ahmad, and William Curtis - they would sit next to me and they were like, ‘You did a number, dude.’ They treated me like a normal person. They tried to normalize the experience as much as possible. Curtis is a mountain biker himself, so he was asking all the questions about where I was or how I did it.”
Chafey says that when he and Stepp first met about five years ago, there was tension over the possibility that Stepp would eventually lose his leg.
But years later, the acceptance of the situation came quickly.
“We both kind of smiled at each other and I said, ‘This is your life and your choice, but at this point, I don’t think this knee is fixable to the degree where you would be able to do the things you want to do,’” Chafey says.
Chafey told Stepp that trying to patch the leg up and fix it could put him in the same place two or three years down the road, and likely every few years thereafter.
“I said ‘Now that you’re cured of cancer and have a whole life ahead of you, do you want this to hold you back or do you want be in a situation where you can just continue on getting stronger and doing as much as you can?’” Chafey says.
Once Stepp made the decision, Chafey and the team helped put their patient at ease over what was going to happen next.
He says Chafey was able to just be present and listen and prepare him mentally for the next chapter in his life, with a new prosthetic that would allow him to be active without pain or the underlying caution he’d been living with.
“What I was thinking about was that I haven’t run in 10 years,” Stepp says. “I was looking forward to getting back to skiing, getting back to cycling. For the past 12 years, since 2008, my leg was a symbol of years and years of pain and the fighting I had gone through with cancer. There were always limitations.
“I knew that was how I was preparing myself, on how amazing it was going to be to do something with no hesitation, no reservation and nothing holding me back.”
Chafey and Stepp continue to have regular conversations and check-ups, predominately virtually. Stepp will be fitted for his prosthetic soon. But he hasn’t stopped. Stepp has been on the ski slopes, cliffs and climbing walls, and of course, the bike.
“In the meantime, Kyle’s been doing a lot of adaptive skiing, so Kyle’s getting out there and living life, which is amazing,” Chafey says. “He never ceases to amaze me.”

Dr. Cheryl Willman to Head Mayo Clinic Cancer Programs
Cheryl Willman, MD, has been named Executive Director of Mayo Clinic Cancer Programs and Director of Mayo Clinic Comprehensive Cancer Center. Mayo Clinic is the nation’s top ranked health care delivery system and hospital.
READ
MORE
CLOSE
Dr. Cheryl Willman to Head Mayo Clinic Cancer Programs
May 17, 2021
Cheryl Willman, MD, has been named Executive Director of Mayo Clinic Cancer Programs and Director of Mayo Clinic Comprehensive Cancer Center. Mayo Clinic is the nation’s top ranked health care delivery system and hospital.
 In her new role, Willman will have full authority and responsibility for Mayo Clinic’s cancer mission (clinical cancer care delivery, research, education and training, and community outreach and partnerships) and will lead the Mayo Clinic Comprehensive Cancer Center programs in Minnesota (Rochester), Arizona (Phoenix/Scottsdale), and Florida (Jacksonville), as well as newly developing Mayo Clinic global cancer programs in London, England and Abu Dhabi, United Arab Emirates.
In her new role, Willman will have full authority and responsibility for Mayo Clinic’s cancer mission (clinical cancer care delivery, research, education and training, and community outreach and partnerships) and will lead the Mayo Clinic Comprehensive Cancer Center programs in Minnesota (Rochester), Arizona (Phoenix/Scottsdale), and Florida (Jacksonville), as well as newly developing Mayo Clinic global cancer programs in London, England and Abu Dhabi, United Arab Emirates.
"Dr. Willman has an outstanding track record of innovation and success as the architect and leader of a National Cancer Institute-designated Comprehensive Cancer Center, serving the needs of the diverse population of New Mexico," said Gianrico Farrugia, MD, President and CEO of Mayo Clinic. "Her accomplishments, experience, and outstanding reputation in the national cancer community make her the right choice to lead Mayo Clinic Cancer Programs and Mayo Clinic Comprehensive Cancer Center."
Willman will join Mayo Clinic in August 2021 from The University of New Mexico, where she has served as the Director and CEO of the UNM Comprehensive Cancer Center for 20 years. Under her leadership the UNM Comprehensive Cancer Center has become one of the most preeminent National Cancer Institute-designated comprehensive cancer centers in the nation.
“Dr. Willman has been a pioneer in cancer care and research, making an incredible impact here at UNM and throughout New Mexico,” said Douglas Ziedonis, MD, MPH, Executive Vice President for Health Sciences and CEO of the UNM Health System. “She is well poised to lead the Mayo Cancer Center to new heights. I am confident in the outstanding leaders at the UNM Comprehensive Cancer Center who will continue the great work that has been achieved under her leadership and help UNM continue a legacy of top-tier patient care, education, research and community outreach.”
Willman and her husband, Ross Zumwalt, MD, a forensic pathologist and former Chief of the New Mexico Office of the Medical Investigator, will maintain faculty appointments and an affiliation with UNM and the UNM Health Sciences Center as they transition to their new roles at Mayo Clinic.
In Service to New Mexico
“My leadership skills have grown through the most enriching experience and challenge in my life: the opportunity to successfully develop a National Cancer Institute-designated
Comprehensive Cancer Center at UNM from “the ground up” in just 15 years,” Willman said.
“With tremendous support from UNM, the State of New Mexico and the communities we serve, we built the cancer center with a clear purpose and an ethical imperative: to assure that all New Mexicans would have access to state-of-the-art cancer treatment and the opportunity to participate in advances in cancer research conducted in a collaborative respectful way, right here in their home state, surrounded by family and friends who love and support them.”
Willman and her team’s strategy took advantage of New Mexico’s opportunities and challenges, including access to the nation’s most advanced science and technology and the challenge of addressing and overcoming overwhelming cancer health disparities in urban and rural communities and tribal nations.
“In our science, we focused on discovering the causes and developing the cures and means to prevent cancers that disproportionately affect the people of New Mexico,” Willman said. “Our clinical mission was to not only develop state-of-the-art cancer diagnosis and treatment facilities at UNM in Albuquerque, but also a statewide collaborative network in partnership with community-based health care systems and cancer practices. In education, we sought to provide opportunities to train members of all of our communities in cancer medicine, research and public health.”

One of the most preeminent NCI-designated comprehensive cancer centers in the nation
When Willman and her team started in 2000, the UNM Cancer Center had 12 cancer physicians in various oncology specialties and $7 million in cancer research funding from the National Institutes of Health, the National Cancer Institute and other agencies. Today, the UNM Comprehensive Cancer Center has 143 board-certified medical, surgical, radiation, gynecologic and pediatric cancer physicians, and 106 cancer scientists who are awarded more than $50 million annually in federal funding for cancer research.
Under Willman’s leadership, the UNM Cancer Center achieved designation and federal funding from the National Cancer Institute in 2005, and in 2015, was designated as one of the nation’s pre-eminent National Cancer Institute-designated comprehensive cancer centers, the highest federal designation status, awarded to only the top 3% of cancer centers in the nation.
“Cheryl Willman is truly a visionary leader and has been a significant agent of change for not only the UNM Comprehensive Cancer Center, but also for our university and the entire state of New Mexico,” said UNM President Garnett S. Stokes. “Her contributions and those of the incredible team she has brought together have helped to shape the world-class cancer care our patients experience today.”
Leading in World-Class Quality Patient Care, innovative Cancer Research and Education
“The UNM Comprehensive Cancer Center has an outstanding leadership team, and I am confident that they will lead the center to new heights and will continue to have a tremendous impact on the people of New Mexico,” Willman said.
Alan Tomkinson, PhD, will assume the role of Interim Director of the Cancer Center and as principal investigator of the Center’s NCI Cancer Center Support Grant. Carolyn Muller, MD, currently Associate Director for Clinical Research, will serve as Interim Deputy Director of the Center’s NCI Cancer Center Support Grant. Zoneddy Dayao, MD, will continue in her role as Deputy Director for Clinical Affairs and Chief Medical Officer, in charge of the center’s cancer care delivery mission.
Willman is a pioneer in the field of cancer precision medicine. Her own research focuses on the use of genomic, next-generation genome sequencing and computational technologies to discovery novel cancer-causing mutations that can be translated to better cancer diagnostics and therapeutics. She co-led the National Cancer Institute's Therapeutically Applicable Research to Generate Effective Treatments Project, also known as TARGET. A component of the NCI Cancer Genome Atlas Project, TARGET focused on genomic sequencing of high-risk leukemias in children and adults.
Through these studies, she and her collaborators discovered novel leukemia-causing mutations more frequently seen in Hispanics and American Indians, providing insights into why these groups had historically failed to respond to treatments developed primarily through studies of non-Hispanic Whites. These discoveries have been translated to several national clinical trials for leukemia sponsored by the National Cancer Institute, leading to significant improvements in patient outcomes.
Continued Collaboration
Willman, her colleagues at the University of New Mexico, and collaborators from the Translational Genomics Research Institute and the Black Hills Center for American Indian Health are now leading one of the nation's National Cancer Institute Participant Engagement-Cancer Genome Sequencing Research Centers.
Through collaboration and partnerships with tribal nations in New Mexico and Arizona, they are focused on discovering the genomic, environmental and behavioral mechanisms underlying cancers that disproportionately affect American Indians and Hispanics, leading to disparities in incidence and outcome. Through culturally respectful community engagement and real-time return of clinical genomic sequencing results to American Indian patients and engagement of communities, they seek to assure beneficence of this work and to improve patient lives. Willman will continue to lead and expand this initiative here at UNM as she transitions to her new role at Mayo Clinic.
About Dr. Cheryl Willman
Willman has been continuously funded by the National Institutes of Health, National Cancer Institute and the Leukemia & Lymphoma Society for more than 30 years. She is a highly cited physician-scientist who has published more than 250 papers, reporting her work in the highest-quality medical and scientific journals.
She also holds 11 patents or patents pending.
She has received numerous awards from the National Cancer Institute, Leukemia & Lymphoma Society, Howard Hughes Medical Institute and W.M. Keck Foundation, among others. She also was a co-founder and president of the Association for Molecular Pathology and is a member of the Department of Energy Women in Science Hall of Fame.
Willman serves on the National Cancer Institute's Board of Scientific Advisors, the Frederick National Laboratory for Cancer Research, the National Cancer Institute-Department of Energy Collaborative Working Group, and the scientific advisory boards of 10 National Cancer Institute-designated cancer centers.
She has received several distinguished public service awards, including the 16th Governor's Award for Outstanding New Mexico Women (2001); the New Mexico Distinguished Public Service Award (2005); the New Mexico La Estrella Award (2013) and the New Mexico Humanitarian Award, 2014. In 2017, she was elected as a fellow of the National Academy of Inventors.
Willman received her medical degree in 1981 from Mayo Medical School, now Mayo Clinic Alix School of Medicine, in Rochester, Minn. She received one of the first Physician-Scientist Awards in 1984 from the National Institutes of Health. Dr. Willman completed her residency and postdoctoral training in pathology and cancer research at Mayo Clinic, The University of New Mexico and the University of Washington.
Undergraduate Pipeline
Health Professions Students Learning to Combine Clinical Medicine & Research
READ
MORE

CLOSE
Undergraduate Pipeline
June 9, 2021
Health Professions Students Learning to Combine Clinical Medicine & Research
Entering University of New Mexico medical student Theodore Muka has long been interested in medicine, but it wasn’t until his mother suffered a stroke that later took her life that he realized the impact the field can have on physicians, as well families.
“I was still in high school when my mother suffered a stroke and the doctor who treated her was a huge factor in my becoming a medical student,” says Muka, a recent graduate of New Mexico State University.
“He was an excellent doctor in providing the treatments my mother needed, but on top of that was the special way he interacted with my family. When she passed away, he came to me personally and did everything he could to answer questions, provide advice and comfort,” Muka remembers.
“Before my mother became ill, I liked the science aspects of medicine. Now I see that the human connection is what really makes it special,” he says.
Spending the summer of 2019 participating in the UNM Undergraduate Pipeline Network Summer Research Program (UPN) gave him ideas for how he can combine research and clinical practice once he becomes an MD, he says.
Muka is interested in cancer research and was excited to be placed in a lab where pediatric cancer research is being conducted at the UNM Comprehensive Cancer Center.
“The experience really made me realize I want to be able to combine those roles, to be a practicing physician involved in research,” he says.
 “The 10-week program has students participate full-time in independent research projects, skill-building workshops and structured collaborative activities,” says Jennifer M. Gillette, PhD, associate professor and senior director for research in the UNM School of Medicine Department of Pathology and director of the UPN program.
“The 10-week program has students participate full-time in independent research projects, skill-building workshops and structured collaborative activities,” says Jennifer M. Gillette, PhD, associate professor and senior director for research in the UNM School of Medicine Department of Pathology and director of the UPN program.
Each undergraduate scholar has a faculty mentor who guides their independent research program. At the end of the 10 weeks, the students present their research project to the scientific community during the program’s competitive poster symposium.
In the classrooms and labs the students work with a host of people, from medical students to faculty members to lab techs, Gillette says.
“Each student has a mentor, but that is just the beginning of their experience,” she says. “Throughout the summer they are going to be interacting with various levels of lab staff, medical graduate students, medical students and pharmacy students. There are a lot of different trainees and labs and various levels.”
Students get to interact first-hand with researchers, Gillette says.
“Undergraduates can ask them questions like, ‘What does your day look like? What decisions did you make to get here?’ The variety of people they interact with shows them that there might be paths other than medical school that will take them to where they want to go,” she says.
“We have people who come in to speak about things like how to create admissions personal statements, resumes. Most years we have also been able to do bonding activities outside of campus, like river rafting and hiking,” she says.
“It really is about skill building for students. What do they need to be successful?”
The number of students each year varies. There were 160 applicants this year from across the country. The program is funded in multiple ways. As an NMSU student, Muka’s participation was supported by New Mexicco IDeA Networks of Biomedical Research Excellence through a National Institutes of Health grant. The program – a partnership of public universities – seeks to build research and educational expertise throughout the state.
“Not only are we giving the students this wonderful exposure and experience, but it allows us also to bring outstanding students from across the state and across the country to UNM,” Gillette says. “It has been a great recruitment tool. At the same time, it has made for a really great experience for everyone.”
Muka agrees.
“I know I want to go into primary care, and I am really interested in pediatrics,” he says. “I want to stay in New Mexico. This has been a wonderful experience for me, and I want to give back as a practicing physician who also works in research.”

To Train a Scientist
UNM Cancer Center Exposes Students to Careers in Cancer Research Thanks to American Cancer Society Diversity Grant
READ
MORE
CLOSE
To Train a Scientist
June 7, 2021
UNM Cancer Center Exposes Students to Careers in Cancer Research Thanks to American Cancer Society Diversity Grant
The University of New Mexico Comprehensive Cancer Center is using a grant from the American Cancer Society to introduce more underrepresented minority undergraduate students to cancer research.
Jennifer Gillette, PhD, leads the Undergraduate Pipeline Network, a program that helps those students with an interest in biomedical research to learn more about their career options. Becoming a scientist requires years of classes and research training, but some students lack access to mentors who can guide their scientific development, Gillette says. The $22,000 Diversity in Cancer Research grant will enable UNM’s Undergraduate Pipeline Network to add four more students.
The 10-week program pairs about 30 undergraduates with UNM faculty mentors. The students work as researchers in a laboratory, write and present their research results, and learn about new employment fields that are developing. For many students, the program offers a first-time glance at the breadth of available work in scientific fields.
“The overall goal of UPN is really to just get students excited about the health professions,” Gillette says.
The students study a range of fields within the biomedical sciences. In its 11 years, the program has gone from two applicants to 160. According to Gillette, more than 95% of the students who complete the program obtain a college degree and more than half continue with further education.
No single grant supports the Undergraduate Pipeline Network. To keep the program running, Gillette partners with several other faculty members to use grants from the UNM Comprehensive Cancer Center, the New Mexico IDeA Networks of Biomedical Research Excellence (INBRE) program, the UNM School of Medicine, the UNM College of Pharmacy, and other sources. The Diversity in Cancer Research grant from the American Cancer Society, which was awarded to Michelle Ozbun, PhD, will fund four students who are interested in cancer research.
Ozbun had previously been awarded an Institutional Research Grant from the American Cancer Society, which is used to help junior faculty establish their research careers. Now she and Gillette will extend the undergraduate program by introducing students to topics in cancer research and by having mentors meet with the students to advise and encourage them throughout the school year.
“The mentors would follow up with a student,” Ozbun says, “to see if they’re facing any barriers, doing research at their university, or thinking about applying for graduate school.”
Gillette says that many students who are interested in science gravitate towards becoming a doctor because that’s a profession — sometimes the only profession — they have heard about in the biomedical sciences. Ozbun adds that some young women believe they can’t become doctors because they’re female.
“It’s exposure,” Gillette explains. “Our goal for the Undergraduate Pipeline Network is to open doors and get students thinking about what other opportunities are out there.”
About the Undergraduate Pipeline Network at UNM
The Undergraduate Pipeline Network summer research experience seeks to cultivate students' interest in research while helping them attain skills needed to apply for and succeed in post-baccalaureate education. The program provides the opportunity for students to choose from several areas of research at the University of New Mexico's Health Sciences Center. The program period covers 10 weeks in the summer and scholars participate in the program a minimum of 40 hours per week. Visit the Undergraduate Pipeline Network webpage to learn more and apply.
About Michelle Ozbun, PhD
Michelle Ozbun, PhD, is a professor in the UNM Department of Molecular Genetics & Microbiology and in the Department of Obstetrics & Gynecology. She co-leads the Cellular and Molecular Oncology Research at the UNM Comprehensive Cancer Center. She has broad background in molecular virology and cancer biology and is an international expert in human papillomaviruses (HPVs), with specific training and 25 years of experience in studying the replicative life cycles of HPVs and carcinogenic progression of HPV-initiated lesions.
About Jennifer Gillette, PhD
Jennifer Gillette, PhD, is an associate professor and Senior Director for Research in the UNM Department of Pathology, and is a full member of the Cellular and Molecular Oncology research group at the UNM Comprehensive Cancer Center. She serves as the Director of the UNM School of Medicine Undergraduate Pipeline Network Program. Her research focuses on hematopoietic stem cell and leukemic cell interactions with the bone marrow microenvironment, focusing on the role of the regulatory scaffold protein CD82.

Assured Resolution
Study of 3D Mammography Shows Fewer Callbacks for New Mexican Women and Greater Confidence in Results
READ
MORE
CLOSE
Assured Resolution
July 8, 2021
Study of 3D Mammography Shows Fewer Callbacks for New Mexican Women and Greater Confidence in Results
For any type of diagnostic test, technology that helps improve the reliability of test results is a welcome addition to a doctor’s arsenal.
So it was with the introduction of three-dimensional tomosynthesis mammography, which allows radiologists and oncologists to see deeper into breast tissues by taking multiple images and allowing specialists to interpret each layer almost as if they were reading a book.
The technology promised greater efficiency at cancer detection and fewer callbacks on patients for whom the interpretation of results was unclear or uncertain.
A recent study by researchers at The University of New Mexico Comprehensive Cancer Center shows that for New Mexican women, at the very least, half of that is true.
The study did two things.
First, researchers combed through more than 35,000 mammograms conducted at UNM Health clinics between 2013 and 2016 and evaluated the frequency with which patients were called back following an initial screening and the numbers of cancers detected by 3D mammography.
The second portion of the study reached out to more than 1,000 women considered at risk to examine their awareness of 3D mammography and what factors were likely to motivate them to pursue the new diagnostic tool.
“I think in this study we added to the national conversation about why 3D is superior and in what ways it can benefit our specific populations,” said Stephanie Fine, MD, a surgical oncologist with the UNM Comprehensive Cancer Center, who led the study.
Fine said the review of the mammography records over the three-year period suggested that women who had 3D breast examinations saw, on average, a 30 percent reduction in the number of callbacks over women who used traditional two-dimensional examinations.
“New Mexico is a poor state and we have a lot of women who would find it difficult to come back for a recall,” she said. “It involves resources these women may or may not have. We don’t know exactly the current numbers for women who fail to come back for a recall or for what reasons. But anything that would decrease the odds that they would have to come back would be a good thing for any state that has resource issues and the poverty levels that we see.”
Fine said that the team noticed that recall rates for traditional screenings actually went up over the course of the years her team studied the records.
“In the last year, it was up to 14 percent as the others went down or stayed the same,” she said.
It is possible that as 3D mammography increased in popularity, radiologists became more comfortable with having a 3D component to the screening to the point that they were less certain of mammograms without them, Fine said.
What Fine’s team didn’t see in the records also was surprising.
“One of the things we thought we would see but we didn’t was a change in cancer detection rates,” she said.
Fine said the number of cancers detected per 1,000 women didn’t substantially change between 3D and more traditional forms of mammography.
“We don’t know why that is,” she said. “Is it because we were in this transition period? Do women in New Mexico have a higher average breast density? The people we captured during those years may have other variables we didn’t uncover.”
Fine said the team was unable to drill down far enough into the data to examine the types of subsets that might lend answers.
Interviews with the 1,000 at-risk patients also led to some interesting conclusions, Fine said. Even in the early days of 3D mammography, most women interviewed had at least heard about the technology. The women may not have heard more than it was considered a superior choice for mammography, but the awareness was there, she said.
“Another interesting finding was that if their primary care provider strongly urged they have a 3D component to their mammogram, that heavily tipped the burden with the patient that she was going to find the resources to make that happen,” Fine said. “It’s a message we hoped to get out that the recommendations of a primary care physician are considered by the patient and they do take that into account.”
Fine said the study was important in that it confirmed the usefulness of 3D mammography at a time when the technology was still emerging. Now, state Medicaid plans cover 3D screenings for women, making it more widely available to New Mexicans and hopefully lowering the number of women who must go through the uncertainty of a recall.
“Even though we didn’t find the increase in cancer detection rates, the recall aspect is really important,” Fine said. “We were able to confirm that that this does work for our community and it does make a difference. That was in the early stages and it might be fun to open that chapter up again and look at more current rates and how it compares to historic controls.”
Brain Cancer: Hunting What’s Left
UNM Cancer Center Scientist Uses $850,000 in Grant Funding to Study How Brain Cancer Makes Its Way Back
READ
MORE

CLOSE
Brain Cancer: Hunting What’s Left
July 12, 2021
UNM Cancer Center Scientist Uses $850,000 in Grant Funding to Study How Brain Cancer Makes Its Way Back
Like a mystery detective, Sara G.M. Piccirillo, PhD, is hunting deadly bad actors by studying the crime scene and questioning bystanders one by one.
But because the bad actors she’s after are brain cancer cells – and because the bystanders are also cells in the brain – Piccirillo must use scientific methods, not police methods, to stop them in their tracks.
An assistant professor at The University of New Mexico Comprehensive Cancer Center, Piccirillo plans to use two grants, a $250,000 grant from the American Association for Cancer Research (AACR) and Novocure and a $600,000 grant from the Ben and Catherine Ivy Foundation, to study tumor cells and cells in the surrounding area, one by one.
“Glioblastoma is very heterogeneous,” Piccirillo explains. “It is not a single disease. It’s a collection of diseases that ultimately end up looking very similar.”
Even within the same tumor, the cells can differ vastly from each other, and these differences are exactly why she thinks the tumors are prone to recurring and what makes them so difficult to fight.
“They will be very heterogeneous in response to treatment,” she says.
Using the two grants, Piccirillo is focusing on residual disease, the cells that are left behind after surgery and survive treatment with chemotherapy and radiation therapy. Doctors cannot know how these cells will behave; some may seed new, aggressive tumors that resist further treatment.
“What is left behind is not equal to what is taken out,” Piccirillo says, so she is developing new ways to search for and treat these residual cancer cells.
To get a sampling of residual tumor cells, Piccirillo previously adapted a fluorescent technology that helps neurosurgeons to find and remove as much tumor as possible during brain surgery. Given as a drink before surgery, the fluorescent molecule is taken in by tumor cells, allowing the neurosurgeon to distinguish tumor from healthy cells.
In previous studies, Piccirillo’s team learned that in 65% of people with glioblastoma, tumor cells reside in a specific brain structure located outside the surgically removed tumor. Using the AACR grant, she and her team will study how cells in this structure behave before and after treatment with chemotherapy, radiation therapy and a new treatment called electric field therapy.
People with brain cancer who are treated with electric field therapy wear a cap studded with electrodes that create an alternating electric field across the brain, which has been shown in clinical studies to markedly slow brain tumor growth.
Piccirillo will use a device to mimic the electric field on individual cells. And she’s planning to conduct genomic and bioinformatics studies on the cells to learn how their behavior changes. She says, “By using genomic studies, we found that this specific area is responsible for the tumor coming back.”
Piccirillo will use the Ivy Foundation grant to study healthy cells called macrophages in the same area.
Macrophages are immune cells, but they don’t normally live in the brain, which has its own security force of immune cells called microglia. Macrophages can enter the brain and play a key role in inflammation.
“Those macrophages have at least two different identities,” says Piccirillo. “They can try to fight the tumor. Or, unfortunately, they can help the tumor to grow.”
Again, using genomic and bioinformatics analysis, Piccirillo will study macrophages and microglia from the area surrounding the tumor to discover whether they help or hinder its growth. She is excited by the newer technologies available at UNM that allow her to conduct this precise cellular analysis. “We didn’t have the opportunity before to dissect a tumor at the single-cell level,” she says.
Piccirillo hopes that her work in studying the heterogeneity of residual brain cancer cells will help to make advancements in treating glioblastoma.
“And if we can do something on this cancer,” she says, “then most likely there will be information useful for other cancers where these features are not so exacerbated.”
About Sara G.M. Piccirillo, PhD
Sara G.M. Piccirillo, PhD, is an Assistant Professor in the Department of Cell Biology & Physiology, and holds a secondary appointment in the Department of Neurosurgery, at the UNM School of Medicine. She is a full member of the Cellular and Molecular Oncology Research Group at the UNM Comprehensive Cancer Center.
Dr. Piccirillo’s research team includes:
Christian Bowers, MD, Assistant Professor and Vice Chair of Clinical Affairs in the UNM Department of Neurosurgery;
Scott Ness, PhD, Professor in the UNM Department of Internal Medicine Division of Molecular Medicine, Associate Director for Shared Resources and Director of the Analytical and Translational Genomics Shared Resource at the UNM Comprehensive Cancer Center; and
Yan Guo, PhD, Associate Professor in the UNM Department of Internal Medicine Division of Molecular Medicine and Director of the Bioinformatics Shared Resource at the UNM Comprehensive Cancer Center.
About the Grants
The content of this publication is solely the responsibility of the authors and does not necessarily represent the official views of the AACR, Novocure or the Ivy Foundation.
About The American Association for Cancer Research
Since 1993, the AACR has allocated more than $480 million and awarded over 890 grants to support thousands of scientists devoted to advancing the understanding, prevention, diagnosis, and treatment of cancer. Our grants support researchers domestically and abroad at every stage of their careers, representing a global commitment to cancer prevention, early detection, interception, and cure. Learn more about the 2020-2021 grants and grantees.
The AACR-Novocure Tumor Treating Fields Research Grant represents a joint effort to promote and support independent investigators who are conducting innovative research focused on Tumor Treating Fields. These grants are intended to provide a deeper understanding of the mechanisms of action of this novel anti-cancer treatment modality and to accelerate the development of new treatment strategies to advance therapeutic options for cancer.
About The Ben & Catherine Ivy Foundation
The Ivy Foundation is the nation’s largest privately funded foundation with a mission of improving survival for people diagnosed with a brain tumor. The Ivy Foundation’s approach is to fund patient focused research in gliomas to improve diagnostics and treatments for patients. Since its inception in 2005, the Ivy Foundation has donated over $100 million to cutting-edge research with the expectation that this will lead to an eventual cure for brain cancer. Learn more at ivyfoundation.org. Follow the Ivy Brain Tumor Center on Facebook, Twitter and LinkedIn.

Change Agent
The UNM Comprehensive Cancer Center Helps Patients With High-Complexity Cases
READ
MORE
CLOSE
Change Agent
July 20, 2021
The UNM Comprehensive Cancer Center Helps Patients With High-Complexity Cases
Elyse Eckart’s journey to The University of New Mexico Comprehensive Cancer Center began, in a sense, with a journey home.
Eckart and her family had been living in California when she and her wife made the decision to come back to Albuquerque.
“Our families are here, and we were missing our extended families and we had small kids,” she said. “We were just tired of living the California life.”
After returning home and finding work as an attorney here, Eckart one day felt a lump in her breast and sought out her primary care physician.
“She agreed that something didn’t feel quite right and sent me along for a biopsy,” Eckart said. “And the whole time everyone was like, ‘Oh, it’s nothing. You’re so young.’ Once I got the diagnosis, I spent some time talking to various people in my circle who worked at both the UNM Hospital and at the Cancer Center and I decided I wanted to be at the teaching hospital at UNM.”
Eckart’s original diagnosis, from another care provider, was hormone-positive invasive ductal carcinoma, a form of breast cancer with a relatively high survivability rate.
“When I switched to UNM, they found an additional tumor and ran biopsies on both and found it was metaplastic, which is a really rare and aggressive form of breast cancer,” Eckart said.
She said that further diagnoses revealed the tumors to be rarer still, with one falling into the triple-negative category, meaning it was negative for estrogen and progesterone receptors as well as for the HER2/neu protein, and the other tumor was hormone positive.
“It was actually a really good thing I ended up at UNM to get a more specific diagnosis,” Eckart said. “In addition to that, my oncologist had me go out to consult with an oncologist at MD Anderson in Houston, because it was a rare cancer and she wanted to make sure the treatment plan she was preparing was blessed by experts in that cancer.”
As an attorney, Eckart is accustomed to researching facts and evidence to answer questions. But with such a rare form of cancer, information was limited and difficult to access. Getting a diagnosis was frightening enough, but trying to find up-to-date information made it more uncertain.
“I think what’s also really scary is it’s hard to find information on it, because it’s really rare,” she said.
“A lot of studies you find don’t talk about the kind of cancer I have and the information that is out there tends to be really dated and is probably a lot scarier than what the actual statistics are today.”
Eckart said she also understands that the nature of statistical studies doesn’t really answer the key questions most individual patients have.
“Stats only relate to the population, not the individual,” she said. “That was a really hard part for me. I just wanted to know what was going to happen to me, and nobody can tell you that.”
In September 2017, Eckart underwent surgery to remove the tumor from her breast, which was followed by six months of chemotherapy and then another five weeks of radiation.
“We had serious conversations about what we would tell the kids and how much we would tell them, and ultimately we decided to be as honest as we could without giving them any information they didn’t need or that would scare them unnecessarily,” she said. “We were very factual with them. We told them I had something called cancer and that meant my cells weren’t acting the way they were supposed to and the doctors would have to give me a bunch of medication to try to get those cells to behave right.
“After that, we stuck to literal facts about how that would impact them: ‘Here are the days I’m going to be sick. Here are the days you’re not going to be able to climb on me.’ For my daughter, the worst part was losing my hair. I think it was a really visible symbol to her that I was sick.”
The conversations never veered into mortality and survivability and Eckart said she was fortunate to receive care from the faculty at the UNM Comprehensive Cancer Center.

Her surgery was performed by Stephanie Fine, MD, and her treatments were coordinated by Zoneddy Dayao, MD. Eckart said the doctors helped explain the complicated terms and procedures to her and helped walk her through the year-long process.
“Dr. Fine literally sat down and drew me pictures,” she said. “When you’re first diagnosed you don’t even know what the jargon is or any of the words people are throwing at you and you have to make pretty quick decisions. Dr. Fine was just amazing at helping me make those decisions. Dr. Dayao was my medical oncologist. She really helped guide chemo and my overall treatment path. She is definitely who I see as the quarterback of my team.”
Eckart said the team really helped her understand the decisions she was making and what their recommendations were and why.
“I never felt like I didn’t have a say but I also felt very informed as to what they thought was the best path,” she said. “They were all really willing to spend time with me to talk through all the ins and outs of a pretty complex process.”
In addition to her treatments, Eckart participated in a clinical trial for a chemotherapy drug. She also has been undergoing hormone therapy, which will end in about a year.
Since her surgery, Eckart has remained cancer-free.
“I have no evidence of disease,” she said. “I think the further out I get from my treatment, the less likely it will be that it returns, but nobody ever says, ‘Oh, you’re cured.’”
Eckart said she has been changed by the experience.
“I think that to some extent, there’s a deep existential transformation that happens when you have any kind of brush with something that can kill you,” she said. “I’ll never say I’m grateful for cancer. It’s not a fun journey, and I wouldn’t wish it on anyone. But I also think it was a big time for personal growth.”
She’s started a new job as a legal counsel for Dell Technologies, working from home. She’s also taken on new physical challenges, going skiing and hiking and doing things she probably would have avoided were it not for her cancer diagnosis.
“The Lobo Cancer Challenge is a great example of that,” she said. “I’ve never been a super athlete but I’m recognizing it’s important to get up and get moving and be active and not worrying about self-image or looking silly.”
Eckart joined the challenge in July 2018 after a meeting with Dayao on her survival plan, following treatment. One of the recommendations was staying active and the event was ramping up and soliciting teams. Eckart joined and dubbed her team “Riders for Racks.” They started with a 25-mile ride and Eckart said she’s considering running the 5K race.
During last year’s virtual event, the team rode 25 miles on the day of the challenge, but Eckart said she got her kids involved and did a hike with them earlier in the month.
Though the team’s nomenclature is inspired by Eckart’s experiences with cancer, she raises funds for the Cancer Center’s Patient Assistance Fund.
Eckart was fortunate to have good insurance that covered her treatment and she wants to do her part to make sure every New Mexican has access to such treatments. She also said that it’s important to support UNM and its position as a social safety net for so many people.
“I think being a cancer patient with relatively curable, lower-stage cancer, you get this ‘Why me?’ feeling, Eckart said. “But on the other hand, you also have what I would term as survivor’s guilt: ‘Why did I get cancer in first place?’ but also, ‘Why am I lucky enough to have something that is relatively manageable, and so far, I’m having a really good outcome when so many people don’t?’
“For me, the other part is if I had to have cancer I’m really glad to have had insurance that I had and I’m really glad to have had access to the Cancer Center and I have a deep moral obligation to pay that forward as much as I can.”

CLOSE
Fun in the Sun
August 30, 2021
UNM Dermatologist Offers Skin Care Tips
Caring for the body’s largest organ – your skin – might seem daunting these days. First, there were the recent sunscreen recalls. Now, with fall’s cooler weather creeping in, you may find your skin getting dry and itchy.
John Durkin, MD, who sees patients at The University of New Mexico Comprehensive Cancer Center and the UNM Dermatology Clinic, offered some tips on keeping skin protected and moisturized in our sunny, arid climate.
Some companies recently recalled sunscreens after finding they were contaminated with benzene, a cancer-causing chemical. Since then, patients have been asking what they should use, Durkin says. He recommends using a mineral-based sunscreen.
“The truth is we are still finding some things out about sunscreen but overall, we still do recommend sunscreen as a means of protection against the risk of skin cancer – both melanoma and non-melanoma skin cancer,”
Durkin says.
Sunscreen protects skin not only from burning but from damage that causes wrinkles and other damage from UV light and the sun.
“Mineral sunscreens aren't absorbed into the skin,” Durkin explains. “They sit on top of the skin. Those sunscreens don't have a negative effect on the coral reef or the environment. We know those sunscreens are generally safe and not harmful.”
Chemical sunscreens, on the other hand, work by actually being absorbed into the skin, he says. Sunscreens that contain oxybenzone or avobenzone are considered chemical sunscreens, he says.
Alternative means of protecting yourself from the sun’s powerful rays can include wearing protective clothing, such as longer sleeves, a wide-brimmed hat and gloves.
“Those are safe ways to protect yourself from the sun, especially if you have concerns over the safety of certain sunscreens,” he says.
He also suggests avoiding spending time outside from 10 a.m. to 5 p.m., when the sun is at its peak, he says. Walks, runs, gardening and other outdoor activities should take place early in the day or in the evening.
A couple of oral supplements may offer protection and can be taken in addition to wearing sunscreen for people who are particularly sensitive to the sun or undergoing treatment for cancer, Durkin says. Nicotinamide, a water-soluble formulation of vitamin B3, and has been shown to decrease the risk of skin cancer. The other supplement that protects skin from UV damage is Polypodium leucotomos, a plant-based antioxidant. But neither should be used as a substitution for wearing sunscreen, he says.
As we move into cooler weather, you may notice that your skin is dry and itchy. Here are some ways to protect it.
Decide which works best for you – ointments, creams or lotions, he says.
Though ointments tend to be the best type of moisturizer, they can also leave your skin feeling greasy.
“The next best thing to moisturize your skin with is a cream,” he says. “Creams tend to be a little bit thicker, absorb better and tend to be less messy.”
For people with sensitivities to fragrances or certain ingredients, he recommends seeking out products that are fragrance-free or labeled as being designed for sensitive skin.
For people who have mildly dry skin, a lotion might work best, he says.
“I think patients who have more severe dry skin would benefit more from a cream or an ointment,” he says.
The No. 1 thing that dries out skin? Taking really hot or long showers. So, he recommends limiting the time and using lukewarm water in the shower. Also, some soaps, especially body washes, can dry out the skin.
Liquid soaps and body washes tend to be more drying, he says. As rule, bar soaps don’t usually dry out skin as much as body washes do, he says. And, using your moisturizer (lotion, cream or ointment) right after showering is the best time to lock in the skin’s moisture, he says.

Sleight of Hand
UNM Scientist Jennifer Gillette Tricks the Bone Marrow into Producing More Stem Cells for Transplantation
READ
MORE
CLOSE
Sleight of Hand
September 16, 2021
UNM Scientist Jennifer Gillette Tricks the Bone Marrow into Producing More Stem Cells for Transplantation
Our bone marrow harbors thousands of rare hematopoietic stem cells – tiny shape shifters that can morph into red or white blood cells. But conditions like sickle cell anemia or immune deficiency can damage these cells, and treatments for blood cancers may destroy them altogether.
To rebuild bone marrow, researchers have perfected the art of transplanting stem cells – either those belonging to the patient or ones that have been donated.
 “You only have so many of these cells,” says Jennifer Gillette, PhD, associate professor in The University of New Mexico Department of Pathology. “These are cells that are with us our entire life. They stay turned off when you’re healthy and things are moving along. But in a stress condition, these are cells that get turned on and rev up and then go quiescent again.”
“You only have so many of these cells,” says Jennifer Gillette, PhD, associate professor in The University of New Mexico Department of Pathology. “These are cells that are with us our entire life. They stay turned off when you’re healthy and things are moving along. But in a stress condition, these are cells that get turned on and rev up and then go quiescent again.”
Gillette has been devising ways to trick donors’ bone marrow into releasing more stem cells into the bloodstream so they can be harvested and transfused.
In a new paper published online in the journal Stem Cell Reports, Gillette and her colleagues describe manipulating a protein called CD82 that sits on the surface of each stem cell and helps them migrate into and out of the bone marrow.
Gillette’s team found that when CD82 disruption is coupled with existing medications used to stimulate stem cell release into the bloodstream, the process is significantly amplified, causing more stem cells to find their way into circulation.
One of those medications – AMD3100 – costs $10,000 for a single dose, she says, and it is hoped that treatment with antibodies might be less expensive.
Patients diagnosed with leukemia or lymphoma may be treated with chemotherapy and/or radiation, which destroy cancerous cells in the bone marrow – along with stem cells.
“It wipes out everything,” Gillette says. “For leukemia or blood cancers you’re trying to get rid of that malignant population and replace it with healthy cells.”
Patients may bank some of their stem cells beforehand for autologous transplants, or they could receive allograft transplants from suitable donors.
“There are some patients that just don’t mobilize well,” she says. “We’re looking for any way that we can enhance cell release, because the number and quality of cells going in really enhance the response of the patients.”
Gillette has applied for a provisional patent to repurpose the antibodies – originally developed to study CD82 functioning – as a clinical treatment. “The next step is to see exactly how that antibody is working,” she says.

UNM Cancer Center Renews NCI Comprehensive Designation
Elite status awarded to New Mexico’s only cancer center designated by the NCI
READ
MORE
CLOSE
UNM Cancer Center Renews NCI Comprehensive Designation
September 21, 2021
Elite status awarded to New Mexico’s only cancer center designated by the NCI

The University of New Mexico Comprehensive Cancer Center has once again been awarded the highest designation and rating in the United States for cancer treatment and research programs.
Comprehensive designation from the National Cancer Institute recognizes the UNM Comprehensive Cancer Center as one of the 51 leading cancer centers in the nation and the only such cancer center in New Mexico.
“We committed to building New Mexico’s finest, most comprehensive center for cancer prevention, research and treatment,” says Cheryl L. Willman, MD. “We have done just that once again.”
Willman led the UNM Cancer Center as director and CEO for 20 years, from initial designation in 2005 and renewals in 2010 and 2015 through this year’s effort. She assumed world-wide leadership of Mayo Clinic’s cancer programs on August 1.

“We are thrilled by this re-designation,” says Alan E. Tomkinson, PhD, interim director and CEO of the UNM Cancer Center. “Comprehensive designation is a testament to the world-class quality of our clinical and research programs. We’re proud to be able to offer the finest cancer care to all New Mexicans.”
Comprehensive designation requires an intensive federal re-certification and designation process every five years. The rigorous process requires the submission of a nearly 1,500-page application followed by an on-site evaluation, which was conducted remotely this year because of the global COVID-19 pandemic.
The application included cancer patient data and outcomes for each person treated at the Center; the development and results of all cancer clinical trials that test new diagnostics and therapies; the results of all laboratory and population-based research; the status of all statewide and national outreach programs and community collaborations; the results of all workforce development and all education and training programs for cancer-trained physicians, nurses, pharmacists, scientists and others; and, the impact of the Center’s programs on its state and region, including economic development and outreach, and addressing the cancer needs and burden of the state.

Douglas Ziedonis, MD, MPH, UNM’s Executive Vice President for Health Sciences and CEO of the UNM Health System, took part in the reapplication process and the NCI’s virtual evaluation.
“We are very proud of our Cancer Center’s faculty and staff and their commitment to excellence, making a difference and helping all New Mexicans,” he says. “The basic, clinical and translational research it conducts, the people it trains, the community outreach it accomplishes and the most advanced cancer care that it offers are vital to our institution and to the people of New Mexico.”
About Cheryl Willman, MD
Cheryl L. Willman, MD, served as Director and CEO of the UNM Comprehensive Cancer Center from 1999 until 2021. She is a Distinguished Emeritus Professor at the UNM School of Medicine. An internationally recognized leukemia researcher, Dr. Willman was named Executive Director of Mayo Clinic Cancer Programs and Director of Mayo Clinic Comprehensive Cancer Center on August 1.
About Alan Tomkinson, PhD
Alan E. Tomkinson, PhD, serves as interim Director and CEO of the UNM Comprehensive Cancer Center. He is a Professor in the UNM Department of Internal Medicine and holds The Victor and Ruby Hansen Surface Endowed Chair in Cancer Research. He also serves as Associate Director for Basic Research at the UNM Cancer Center. Dr. Tomkinson is an international expert in the DNA repair mechanisms that prevent cancer by maintaining genome stability and in understanding how these pathways are perturbed in cancer cells. His work is leading to the development of new therapies which target these alterations in cancer cells.
About Douglas Ziedonis, MD, MPH
Douglas Ziedonis, MD, MPH, has served as Executive Vice President for UNM Health Sciences and CEO for the UNM Health System since December 1, 2020. He has breadth of experience and has held leadership roles at academic institutions as varied as the University of California, San Diego, UCLA, UMass, Yale University and Rutgers, and he has conducted extensive work with diverse populations, including Indigenous communities. Additionally, he is a Distinguished Professor whose own medical and public health research and leadership impact continues to address health disparities – including issues such as cancer prevention, homelessness, mental illness and addiction – and being a champion for diversity and inclusive excellence.
Three Steps Forward
Three-Time Hodgkin Lymphoma Survivor Thrives Following a Stem Cell Transplant at UNM Comprehensive Cancer Center
READ
MORE

CLOSE
Three Steps Forward
September 23, 2021
Three-Time Hodgkin Lymphoma Survivor Thrives Following a Stem Cell Transplant at UNM Comprehensive Cancer Center
 The foundation of any dance is putting the body into motion.
The foundation of any dance is putting the body into motion.
There’s the first step, followed by another and another until the individual pieces blend into a larger theme or a greater story.
Mariah Candelaria’s story has included dancing since she was a little girl, all the way to adulthood as a three-time cancer survivor.
“Dancing is definitely in my blood – music and singing,” Candelaria said. “I danced with my cousin since we were little. We used to do Folkloricio and dancing at fairs and stuff like that. And when we were older, we also taught a class together, which was a Zumba class. We wanted to lose weight and get in shape and help other people feel good about themselves. That’s kind of the route we took.”
Candelaria’s life would be interrupted not once, not twice, but three times by Hodgkin lymphoma.
“The first time it happened was in 2008 and I was actually in nursing school at the time,” she said. “I was learning a lot in general medically and I started to notice pain while I was sleeping in the area of my armpits.”
Candelaria was also experiencing night sweats, something that hadn’t happened before, as well as dry, itching skin. Because of the area where the pain was, she had it checked immediately. But it wasn’t until doctors took a biopsy that they determined she had cancer.
“The reason why I noticed it more was because it was uncomfortable when I was dancing,” she said. “There were certain moves where I was like, ‘Hey, why is this hurting?’”
For her first fight with Hodgkin lymphoma, Candelaria said she underwent five months of chemotherapy treatment.
Candelaria said the experience was a difficult because it interfered with her normally active lifestyle.
“The minute you start feeling better you’re going back for the next round,” she said. “It’s hard to keep your spirits up and it’s hard to be positive. It’s important that whatever it is that keeps you positive to keep doing it. Some people like to knit. Some people like to do art. Some people like to dance and exercise, meditate or whatever. I feel like it’s important to have some sanity in your life and less stress.”
Candelaria’s first relapse came a few years later, shortly after the birth of her second daughter.
“Right after I had her I started noticing pain again, and this time, I actually felt a lump above my clavicle,” she said. “It felt like a pretty big ball and it was pretty evident it was back.”
Candelaria speculates that her pregnancy might have triggered the relapse. Perhaps the stress of it all, or the hormonal changes of pregnancy contributed. But her newborn was a blessing and an anchor to keep her focused during another three months of chemotherapy, followed by 15 days of radiation treatment.
“I didn’t have a choice to feel too sick to get up that day,” she said. “My kids kept me going.”
Candelaria’s second relapse happened in 2019 after she was in a car accident.
“It caused a lot of pain in my right arm and affected my legs,” she said. “It kind of knocked me out, and I couldn’t do dance for a while. It was hurting my legs so bad and it just caused a lot of depression. Not being able to move my body left me in a bad state. Then I got really sick that November. I started getting the night sweats again and I felt the pain in my right armpit, and I knew right away.”
Her third round of treatment would take a different turn.
Candelaria chose to undergo a stem cell transplant.
The process coaxes bone marrow cells into a patient’s bloodstream where stem cells can be harvested and then stored. It allows for patients to receive intense chemotherapies that are damaging to bone marrow.
But once the chemotherapy treatments are finished, the stored stem cells are returned to the patient’s bloodstream where they can go back into the bone marrow and grow new blood cells.
Candelaria said after initially beginning the process at another cancer center, she decided to come home to The University of New Mexico Comprehensive Cancer Center to finish her treatment.
She said she owes a big part of her success to the support she felt from UNM Comprehensive Cancer Center providers and staff, including Matthew Fero, MD, and Karen Miller, MD, who is now retired.
“There were certain things Dr. Fero would ask me to do and I would not do them,” she admitted. “He would still – no matter how bad I felt, if broke out in rash or was hurting really bad – I would shoot a text and there was always open communication. I really feel like it helped during treatment.”
Candelaria was at UNM Hospital for 17 days and experienced painful complications from the treatments.
“My body reacted to my own cells as if they were from a donor,” she said. “When I swallowed anything, it felt like glass.”
But Candelaria was determined to stay active even during her stay. Her parents would bring her two daughters to visit and she asked hospital staff to provide her with something she could use to exercise.
They provided her with a foot pedal machine. She used that or would go for walks and try to sing.
“I really did want to stay in bed,” she said. “My heart was racing just sitting there. But I would force myself to get up and force myself to walk and force myself to eat something – at least do something I could do to feel better.”
After she was discharged Candelaria found her way back to dance – it took about a week – including a local DanceFit group she had been a part of before her chemotherapy.
Candelaria said she continued to keep in touch with Fero following her discharge.
“I would send pictures and tell him, ‘Look at my progress,’” she said. “I wanted to prove that part of it is mind over matter, and yes, you feel horrible when you feel sick, but if you let yourself feel horrible, you’re going to. If you find other ways to distract you from that, it at least helps a little bit. If you have multiple things, even better.”
Candelaria wants to give back after her experience. She said she wants to rely on her personal fight with cancer and her nursing education to provide a class to others who are going through Hodgkin lymphoma.
She is also a participant in the Lobo Cancer Challenge, which raises money for cancer research and treatment at the UNM Comprehensive Cancer Center. This year, since the event is virtual, she is organizing a raffle and working with other gyms and fitness clubs to hold events or offer prizes.
“That’s what I feel my purpose is now to help people going through stuff like this, because it’s not easy,” she said.
She’s also taking life as it comes, from moment to moment, beat-to-beat, step-to-step.
“I lost a lot of muscle. I lost a lot of weight,” she said. “I lost a lot of things; my hair twice, during that process it was really horrible and gratefully I’m doing a lot better. I’m dancing more than I ever have, working out more than I ever have.
“I’m the kind of person who is really spontaneous and lives in the moment. I realize the value of life, especially after going through it so many times. People worry about such tiny little things every day and it really doesn’t matter. You have to appreciate things, because if you don’t what’s the point of living?”
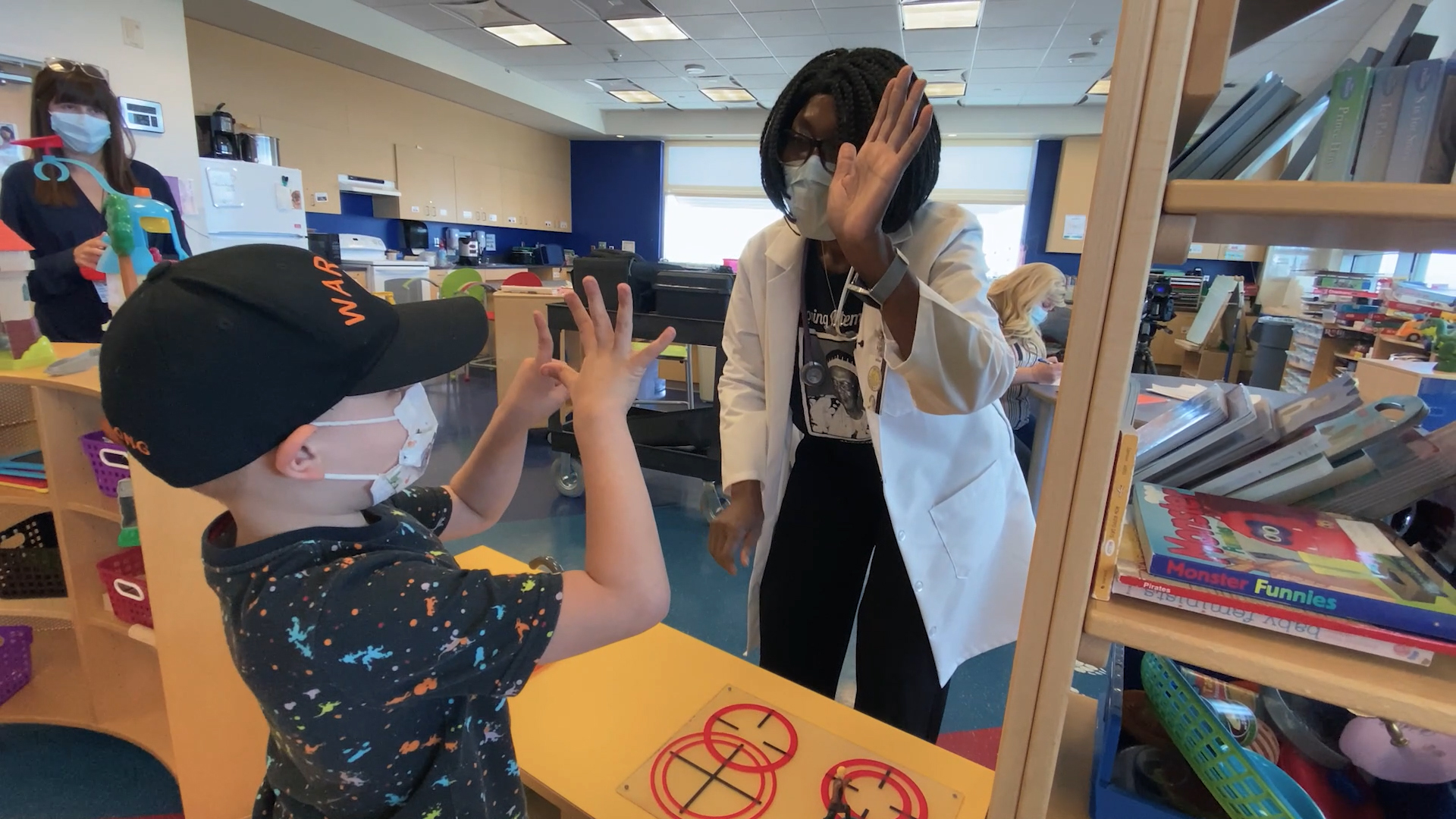
CLOSE
Care Commitment
September 22, 2021
UNM Providers and Staff Join in Childhood Cancer Awareness Month
September is Childhood Cancer Awareness Month, a reminder that each year nearly 16,000 children aged 0 to 19 are diagnosed with the disease each year – approximately one in 285 U.S. kids.
“Here at UNM we try to celebrate it every year,” says Koh Boayue, MD, associate professor of Hematology and Oncology in The University of New Mexico School of Medicine, who treats many of these children. “We hope that year-long we can do things to raise awareness for these children and their families who are going through these difficult times.”
Check out these videos to learn more about how UNM doctors, nurses and staff are providing state-of-the-art cancer care and helping children and their parents navigate the challenges they face:
Hunter
Makayla

Testing Troubles
UNM Researchers Find Cervical Cancer Screening is Overused – and Underused
READ
MORE
CLOSE
Testing Troubles
October 11, 2021
UNM Researchers Find Cervical Cancer Screening is Overused – and Underused
Cervical cancer screening saves lives — no one disputes that.
But University of New Mexico researchers have found that many women are screened too often, leading to unnecessary procedures that may carry their own harms, while some women are not getting tested often enough, putting them at higher risk for poor outcomes.
 The team led by Cosette Wheeler, PhD, Regent’s Professor in the UNM Department of Pathology and director of the Center for HPV Protection at the UNM Comprehensive Cancer Center, looked at compliance with updated national guidelines for cervical cancer screening issued in 2012.
The team led by Cosette Wheeler, PhD, Regent’s Professor in the UNM Department of Pathology and director of the Center for HPV Protection at the UNM Comprehensive Cancer Center, looked at compliance with updated national guidelines for cervical cancer screening issued in 2012.
The new recommendations for women aged 30-64 at average risk for cervical cancer called for co-testing for human papillomavirus (HPV) and liquid-based cytology – an updated version of the traditional Pap smear – every five years, or every three years for cytology alone.
The researchers studied statewide data collected by the New Mexico HPV Pap Registry, established in 2006 to evaluate cervical-cancer screening delivery, and report in the Journal of the National Cancer Institute that 65 percent of New Mexico women screened in 2019 with a normal prior co-test had undergone re-screening within the previous three years – far more often than recommended.
At the same time, 6.5% of women screened with a prior negative co-test and 14.9% of women with a prior negative cytology alone were not re-tested for more than five and up to seven years. These findings were concerning, given that negative cytology alone does not provide the same assurance that a negative co-test does for having a low risk of cervical cancer.
“We not only show the overuse of cervical cancer screening, but we also show that more and more women are not coming back for more than five years,” Wheeler says.
“Alarmingly, as recommendations for intervals between cervical screening have become longer and therefore less frequent, more women are falling out of screening within reasonable and recommended intervals. They are not coming back until five or more years, which is too long to have protection from prior screening.”
Over-testing is problematic not only because HPV tests are expensive, but because a positive result does not necessarily indicate a problem. An estimated 40 percent of women aged 18-59 years are infected with one or more genital HPV types, but most infections will go away on their own and do not pose a cancer risk, Wheeler says.
“What you’re trying to do is only detect those HPV infections that will cause or reflect existing disease,” she says, but follow-up biopsies to resolve that question add expenses, and if additional tissue removal is required, it may increase the risk for reproductive harms, including pre-term delivery.
Under-screening poses is the worst-case scenario, because a woman may have started to develop undetected cancer if she has gone too many years without appropriate screening, Wheeler says, and inequities in screening, including race, ethnicity and being economically and socially disadvantaged, can contribute to increased cancer risk and reduced access to health care.
Part of the problem lies with long-standing recommendations that women receive a Pap screen every year. From a scientific standpoint, “women of average risk, regardless of age, should not get a cervical screen more than once every three years,” Wheeler says. But the routine screening was at least easier to keep track of when done annually.
She suggests that performing screening more often than recommended with co-testing every one, two or three years has financial benefits for both clinicians and laboratories, which is another dimension of the problem.
Now, doctors – and their patients – may not do a good job of keeping track of when the last screening was performed, and women often change where they receive health care. Meanwhile, centralized tracking systems to help providers and patients keep track of when women should schedule a five-year co-test or three-year cytology are mostly lacking in the U.S.
The New Mexico HPV Pap Registry, with its statewide reach, is an exception, Wheeler says. “Systems like this could be used to help providers deliver cost-effective screening and timely follow-up of abnormalities,” she says.
“Estimates for cervical cancer prevention in the U.S. were in the ballpark of $8 billion a year prior to the implementation of HPV vaccines, which represent significant additional costs,” Wheeler adds. “There is little ability to assess whether clinical guidelines are being followed or if there are positive or negative impacts of guideline practices in real-world settings. That’s the way the New Mexico HPV Pap Registry is contributing.”
Prescription Precision
On the surface, the pharmacy at The University of New Mexico Comprehensive Cancer Center looks pretty familiar.
There’s the counter, the shelves and the helpful faces working with customers.
But a retail pharmacy is just one part of a larger operation that is integrated into nearly every function of the UNM Comprehensive Cancer Center’s clinical operations.
READ
MORE

CLOSE
Prescription Precision
November 23, 2021
On the surface, the pharmacy at The University of New Mexico Comprehensive Cancer Center looks pretty familiar.
There’s the counter, the shelves and the helpful faces working with customers.
But a retail pharmacy is just one part of a larger operation that is integrated into nearly every function of the UNM Comprehensive Cancer Center’s clinical operations.
Pharmacists work with oncologists and oncology nurses to make sure chemotherapy dosages are correct for patients undergoing treatments at the center, while the team of pharmacists in the retail side work to make sure patients understand the medications they’re taking home – and even look for ways to help them pay for it.
“In our retail pharmacy, we help everyone who comes in the door for any prescription or over-the-counter medication,” said pharmacy director Nick Crozier. “In addition, we help all oral oncology patients, no matter where they fill their prescriptions. We do an initial consultation and go in depth about what to expect and then we follow up with the patients to make sure everything is OK.”
Oncology drugs can be complicated and expensive. The pharmacy team makes sure patients understand what they are taking and helps them make their way through the insurance process as well.
“Not only does the pharmacy staff deal with insurers, a big part of what we do is we look for additional funding for patients without insurance, or who need help with co-pays,” Crozier said.
It takes a dedicated team of professionals, many of whom have undergone specialized training to become board certified in oncology pharmacy.
 Pharmacists and technicians work together to make sure the dosages provided to patients who receive treatment at the Comprehensive Cancer Center’s clinics are safe and effective.
Pharmacists and technicians work together to make sure the dosages provided to patients who receive treatment at the Comprehensive Cancer Center’s clinics are safe and effective.
Chemotherapy treatments can require combinations of drugs, and the communication and documentation of what goes into the mix is absolutely crucial, Crozier said.
“The inventory just has to be absolutely perfect, otherwise we may not be able to treat a patient on the day they are due,” he said.
Every detail of the medication order is scrutinized so that the medication order that’s sent to the technician for mixing is completely accurate, Crozier said.
Technicians undergo specialized training as well, including learning the proper order in which to mix certain drugs.
“There are unique things that a tech needs to know to work in oncology, and it usually takes about six months,” Crozier said.
If a drug isn’t mixed properly, it often must be thrown away, because each dose is unique for a patient.
But even before a patient comes in for treatments, the Comprehensive Cancer Center’s pharmacists are involved in that patient’s care, working with oncologists to determine which drugs might work the best.
“When they’re working downstairs with the doctors, they’re looking at the disease state, prior lines of therapy and the tumor markers,” Crozier said. “They help pick the right drug regimen for the patient.”
When patients come in for their treatments, pharmacists are behind the scene helping determine if it’s appropriate for them to receive treatment that day based on the patient’s laboratory test results. Pharmacists also rotate in the UNM Hospital inpatient cancer unit, because many cancer treatments require hospital stays.
As a part of the UNM Health Sciences Center, the Comprehensive Cancer Center also offers educational opportunities, including a one-year oncology residency for pharmacists looking to expand their knowledge before entering the workplace.
CLOSE
Vital Vigilance
November 30, 2021
Lung Cancer Awareness Month Highlights Early Screening to Save Lives
Of all the cancers that kill hundreds of thousands of people every year, lung cancer is the deadliest, says Akshu Balwan, MD, attending physician at The University of New Mexico Hospital and assistant professor in the Division of Pulmonary & Critical Care in the UNM School of Medicine.
Early screening is essential to saving lives, Balwan says.
UNMH is using new technology to screen patients who have a suspected lung cancer diagnosis. The robotic bronchoscopy machine can help perform biopsies of nodules – small spots of suspicious tissue in the lungs that might not be visible through conventional bronchoscopy.
It increases a pulmonary physician’s capability to biopsy lung nodules that are small and deeper in the lung, Balwan says. “This will help us diagnose cancer at an early stage, at which point it is more likely to be curable. It also opens opportunities toward using this advanced technology for possible novel curative therapies.”
The new robotic bronchoscopy device at UNMH – the only one in the state – is a large machine that takes up a good amount of space in an operating room. One part of it looks like it could be part of a gaming console, but this machine goes way beyond, creating a 3-D map of the lungs.
Fewer than 10% of people who are eligible for screening get screened, and as part of Lung Cancer Awareness Month, Balwan and his team hope to change.
Who should get screened? Anyone who smokes or has smoked cigarettes in the past should check with a primary care provider.
“Research shows that we can decrease the number of deaths upwards of 20% with lung cancer screening,” Balwan says. “The problem with lung cancer is 80% of it is diagnosed in the late stages.”
UNM’s interventional pulmonology program has continued to evolve and establish itself as the largest, most comprehensive interventional program in the state, he says.
“We’ve made great advances in treatment of lung cancer, and also have found ways to detect lung cancer early with lung cancer screening,” Balwan says.
Some symptoms of lung cancer, according to the Lung Cancer Research Foundation, are:
